Members of the Duke Neurology Department did their part for Stroke Awareness Month, contributing to eight new peer-reviewed studies published this May. But our other divisions didn’t hold back either, with thirteen other articles advancing our understanding of neuro-oncology, multiple sclerosis, headache, and other subjects.
Read about each of the studies published from members of the Duke Neurology Department below, and find links to the original journal articles as well.
Stroke
- Brian Mac Grory, MB BCh, MRCP, and Wuwei “Wayne” Feng, MD, MS, were the senior authors of an analysis of current approaches and future directions of structural and functional imaging of the retina in central retinal artery occlusion. Pratik Chhatbar, MD, PhD, Taewon Kim, PhD, and Mary Guhwe, DNP, FNP-BC, also contributed to the study, which appears in the Journal of Cerebrovascular Disease. Read that study here.
- A new study raises potential concerns about prescribing oral anticoagulation (OAC) after an ischemic stroke for older patients with heart failure without atrial fibrillation. A team including Shreyansh Shah, MD, and Ying Xian, MD, PhD, examined outcomes of patients with a history of heart failure who were initiated on OAC during a hospitalization for an acute ischemic stroke. Patients receiving OACs had a greater risk of death, bleeding and re-hospitalization without an associated reduction in recurrent ischemic stroke. Read the study in the Journal of Cardiac Failure.
- Randomized trials have already demonstrated the benefit of dual antiplatelet therapy in patients with minor ischemic stroke or high-risk transient ischemic attack. A team including Brian Mac Grory, MB BCh, MRCP, examined whether carotid stenosis was associated with increased risk of ischemic stroke and whether clopidogrel and aspirin were superior to aspirin alone for this group. Their analysis found that carotid stenosis was associated with increased risk of ischemic stroke during follow-up, but no significant differences in outcomes for added clopidogrel in patients with versus without carotid stenosis. Read the full article in Stroke.
- People presenting with mild symptoms of stroke are an underrepresented population in clinical trials. A new study in Stroke examines multidimensional outcomes, predictors of worse outcomes, and effects of thrombolysis in this population. Brian Mac Grory, MB BCh, MRCP, contributed to that article, which is available here.
- Some ischaemic stroke patients with atrial fibrillation (AF) have ischaemic stroke despite anticoagulation. A team including Brian Mac Grory, MB BCh, MRCP, analyzed the association between prestroke anticoagulant therapy and recurrent ischaemic events and symptomatic intracranial haemorrhage, finding that AF patients with ischaemic stroke despite anticoagulation may have higher recurrent ischaemic event risk compared with anticoagulation-naïve patients. Read the full study in the Journal of Neurology, Neurosurgery & Psychiatry.
- In the same publication, Mac Grory also contributed to a literature review of lancular stroke, a marker of cerebral small vessel disease and accounts for up to 25% of ischaemic strokes. Their analysis suggests that lacunar stroke is a heterogeneous disease with various mechanisms, including most commonly lipohyalinosis and less commonly atheromatous disease and cardioembolism, highlighting the importance of a careful review of brain and neurovascular imaging, a cardiac and systemic evaluation. Read that article here.
- A new systematic review and meta-analysis examines the effectiveness and safety of dual antiplatelet (DAPT) therapy with P2Y12 inhibitors (clopidogrel/ticagrelor) and aspirin versus aspirin monotherapy in patients with mild ischemic stroke or high-risk transient ischemic attack. Ying Xian, MD, PhD, contributed to that study, which appears in Stroke.
- Postdoctoral associate Taewon Kim, PhD, wrote a letter discussing critical research insights in motor learning in stroke based on the neural mechanism of the interleaved practice format. Read that analysis in the Journal of Exercise Rehabilitation.
Neuro-Oncology
- A new study by first author Jennifer Kang, MD, Katherine Peters, MD, PhD, and colleagues from the Departments of Neurosurgery and Medicine answers important questions about the potential benefits of palliative care for critically ill patients with brain metastases. The team compared mortality rates, discharge to hospice rates, and services provided by palliative care for brain metastasis patients who received consults to those who did not, finding that palliative care was an underused service that offers potential benefits for symptom management and decision-making. Read that study in the Journal of Pain Symptom Management.
- Peters also contributed to global assessment of the state of neuro-oncology during the COVID-19 pandemic. Their analysis examined clinical practice, research environment, institutional preparedness and impact on patients from 21 neuro-oncology organizations across six continents. Read that analysis in Neuro-Oncology Advances.
Headache
- Headache fellow William Coleman, MD, and Sweta Sengupta, MD, discuss a recent patient case involving visual snow treated with phenylephrine. Read that case report in Headache.
Neuroscience
- Leonard White, PhD, led an effort to create a high-resolution (50-200μm) interactive 3D atlas of the human brainstem, built after scanning a complete postmortem brainstem with MRI for 208 hours. Read the article published in NeuroImage or view the complete interactive atlas here.
- A new cross-sectional survey examines how the treatment preferences of older adults with mild cognitive impairment compare to those with normal cognition. Brenda Plassman, PhD, and Kathie Welsh-Bohmer, PhD, contributed to that study, which appears in the Journal of General Internal Medicine. Read that study here.
Multiple Sclerosis and Neuroimmunology
- Mark Skeen, MD, wrote a series of three essays discussing new directions in the treatment of multiple sclerosis in the Journal of Clinical Neurophysiology. The first, written with the University of Miami’s Luca Pani, MD, discusses regulatory issues involving biomarkers and surrogate end points in MS trials. The second discusses how clinical neurophysiology will influence changing paradigms and unmet needs in MS, and the third discusses the use of evoked potentials in MS clinical trials. biomarkers and surrogate end points in MS trials, changing paradigms and clinical neurophysiology and the use of evoked potentials in MS clinical trials. Read those articles here.
Neuromuscular Disease
- Lisa Hobson-Webb, MD, was the senior author of a Muscle and Nerve editorial that discusses quantitative muscle echointensity as a practical technique that uses ultrasound to evaluate children with suspected neuromuscular disorders. Read that article here.
- While amyotrophic lateral sclerosis (ALS) is primarily a neuromuscular disease, evidence increasingly points to it also affecting other body systems, affecting cognition, sleep, behavior, pain, and fatigue. A team including Rick Bedlack, MD, PhD, reviewed these non-motor effects, current treatment options and topics for future research in the latest issue of CNS Drugs. Read that article here.
- Jeffrey Guptill, MD, MHS, contributed to a study providing guidance for clinicians treating patients with myasthenia gravis via telemedicine visits, including offering the myasthenia gravis core exam. Read that study in Muscle and Nerve.
Translational Brain Sciences
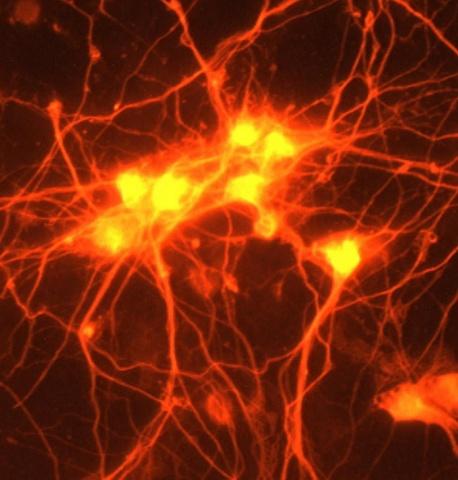
- Ornit Chiba Falek, PhD, was the senior author of a study that found an attractive therapeutics target for gene therapy in patients who suffer from synucleinopathies such as Parkinson’s and dementia with Lewy body: the SNCA intro 1 CGI region. The Chiba Falek lab’s Julio Barrera and first author Jeffrey Gu also contributed to the study, which appears in Frontiers in Neuroscience. Read it here.