Members of the Duke Neurology Department got the new year off to a fast start this January, contributing to 10 new peer-reviewed journal articles. Rick Bedlack, MD, PhD, was the senior author of three new publications investigating potential new therapies for amyotrophic lateral sclerosis (ALS). In addition, faculty from our division of Memory Disorders investigated a new form of retinal imaging that may be able to identify signs of Alzheimer’s before symptoms appear, and Neurocritical Care Fellow Gabriel Torrealba-Acosta, MD, helped design a checklist that improved the delivery of neurocritical care. Read about these and other recent publications, and find links to the original research articles themselves, in the paragraphs below.
Memory Disorders
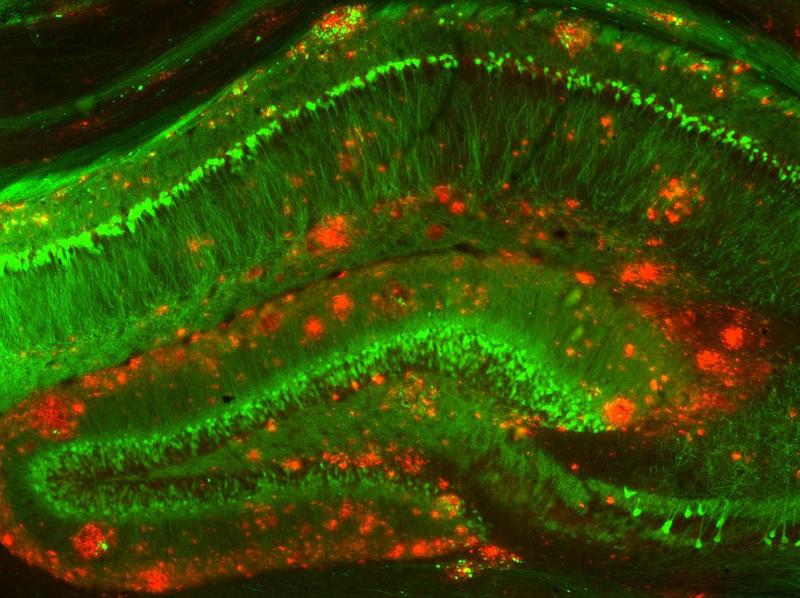
- Neurodegenerative diseases such as Alzheimer’s cause small, measurable differences to the retina years before symptoms appear, making images of this area a potential source of early biomarkers. Kim Johnson, MD, and Andy Liu, MD, MS, were part of a team that assessed the presence of these abnormalities in Alzheimer's dementia and mild cognitive impairment (MCI) using ultra-widefield (UWF) retinal imaging. Their pilot study found statistically significant differences in the retinal vasculature in peripheral regions of the retina among the distinct cognitive stages. Read their full study in Translational Vision Science & Technology.
- Brenda Plassman, PhD, contributed to a new longitudinal analysis that answers important questions about loneliness, sensory impairment, and cognitive decline in older adults. Plassman and colleagues analyzed data from the Health and Retirement Study (HRS) and The Aging, Demographics, and Memory Study (ADAMS), finding that loneliness moderated but did not mediate the association between visual impairment and the rate of cognitive decline, and that both vision and hearing impairment were significantly associated with increased severity of loneliness. Read the full study in Frontiers in Neuroscience.
Neuromuscular Disease
- In the 69th entry in the ongoing ALS Untangled series, senior author Richard Bedlack, MD, PhD, and colleagues examined the potential for astaxanthin as an alternative treatment for ALS. Their analysis found a theoretical mechanism for the medication as well as one potential ALS reversal related to its use. Read their full analysis in Amyotroph Lateral Scler Frontotemporal Degeneration.
- Senior author Rick Bedlack, MD, PhD, Xiaoyan Li, MD, and former Duke neuromuscular fellow Yuyao Sun, MD, conducted a review of the pharmacology and clinical trials evaluating sodium phenylbutyrate and/or taurursodiol among people living with ALS. Read their article in Expert Review of Neurotherapeutics.
- Rick Bedlack, MD, PhD, was also the senior author of a study that sheds light into the role cerebrospinal fluid (CSF) plays in the development of ALS. Bedlack and colleagues filtered CSF from 11 ALS patients and then injected groups of mice with saline, filtered ALS-CSF, or unfiltered ALS-CSF. They then identified proteins implicated in ALS pathogenesis, showed that filtration reduced those proteins, and found that mice receiving them had reduced mobility, demonstrating that CSF filtration these were removed in significant amounts could be a novel solution for patients suffering from this deadly and irreversible condition. Read the full article in Cureus.
- Lisa Hobson-Webb, MD, was part of a team that implemented a rotational 3-D shear wave elasticity imaging (SWEI) system that measures the shear wave speed both along and across the fibers in a single 3-D acquisition, with automatic detection of the muscle fiber orientation. Their results suggest using 3-D SWEI has the potential to improve the precision of SWEI measurements in muscle. Read the full article in Ultrasound in Medicine and Biology.
Neurocritical Care
- Neurocritical Care Fellow Gabriel Torrealba-Acosta, MD, was part of a team that designed and tested a systematic safety checklist for providing neurocritical care. The team designed a checklist using a Plan-Do-Study-Act methodology and applied it to 400 patients. Implementing this checklist resulted in shorter lengths of stay and reduced infections. Read that article in BMJ Open Quality.
Stroke and Vascular Neurology
- Jamila Minga, PhD, was the senior author of a study that examined racial/ethnic differences in communication after right hemisphere strokes in a group of Black and white women, finding Black women tended to ask fewer questions of all types in conversation post-stroke. Read more about these findings in the Journal of Speech, Language, and Hearing Research.
- Recent vascular Neurology Fellow Alok Sahgal, MD, and Brad Kolls, MD, PhD, were the senior authors of an article that examined whether information available during acute care telestroke consults could identify hemorrhagic stroke patients patients who could remain at local centers for care rather than requiring specialty neurosurgical interventions. Their retrospective examination of 116 hemorrhagic stroke patients found that coupling the ICH and GCS scores could provide reliable triage guidance for identifying patients for retention at the referring center. Former vascular neurology fellow Imran Farooqui, MD, also contributed to the article, which appears in the Journal of Stroke and Cerebrovascular Disease. Read it here.
Other Topics
- A new case report describes the clinical characteristics of three older adults aged >65 years with cognitive difficulties prior to their COVID-19 infection who reported worsening of neurocognitive symptoms in the convalescent COVID-19 phase. Senior author Andy Liu, MD, MS, Simon Davis, PhD, Thomas Farrer, PhD, and colleagues hypothesize that the persistent inflammatory or immune response in the convalescent COVID-19 stage, more commonly referred to as the indirect mechanism, contributes to the clinical syndrome known as the Post-Acute Sequelae of SARS-CoV-2. Read that article in the Journal of Covid Research and Treatment.