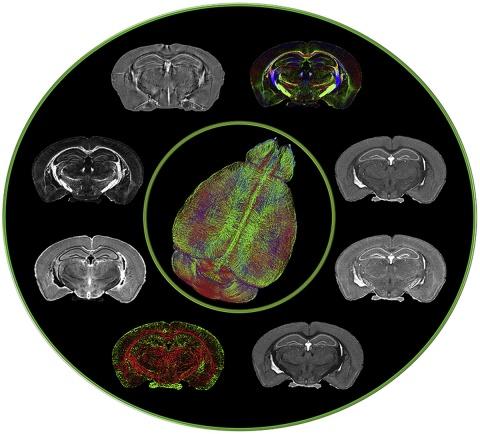
Members of the Duke Neurology Department continued to advance the fields of clinical and translational neuroscience this April. Our faculty contributed to the first major systematic review of self-management programs for epilepsy, helping to answer questions about what makes these programs more or less effective. Another article discussed the benefits of CN-105, a therapeutic agent that may help reduce the harmful neuro-inflammatory response associated with stroke, traumatic brain injury, and other conditions. And Leonard White, PhD, helped create the highest-ever resolution photos taken of the brain using MRI (photo, right). Read more about each of those articles, and find links to the original journal entries, below.
Epilepsy
- Self-management programs offer enormous potential for helping patients better control their epilepsy, but the data on the effectiveness of these programs, and what makes them effective, are limited. Matt Luedke, MD, Aatif Husain, MD, Tung Tran, MD, Saurabh Sinha, MD, and colleagues conducted the first major systematic review of this field, offering a look into factors that make people more or less likely to adopt or benefit from these programs. Read that article here.
Neurocritical Care
- Apolipoprotein E (apoE), a protein produced in the brain that modulates the neuroinflammatory response during acute brain injury, holds potential as a therapeutic target to reduce the secondary impact of brain injury. In the latest issue of Neurotherapeutics, senior authors Michael “Luke” James, MD, and Daniel Laskowitz, MD, MHS, and Haichen Wang, MD, and neurocritical care fellow Jordan Komisarow, MD, discuss the apoE mimetic peptide, CN-105, which has demonstrated efficacy across a wide variety of preclinical models of brain injury and safety and feasibility in early-phase clinical trials. Read that article here.
Neuromuscular diseases
- In response to the COVID-19 pandemic, Jeffrey Guptill, MD, MHS, and other global experts in myasthenia gravis formed an international working group and offered their guidance about concerns related to COVID-19 in patients with myasthenia gravis and Lambert-Eaton myasthenic syndrome. Read their recommendations in the Journal of the Neurological Sciences.
Translational Brain Sciences
- Postoperative delirium is a common complication in many older adults and in patients with dementia including Alzheimer's disease (AD). The course of delirium can be particularly debilitating, while its pathophysiology remains poorly defined. In the latest issue of Alzheimer’s and Dementia, Carol Colton, PhD, and colleagues evaluate the relationship between postoperative immune and neurovascular changes and the pathogenesis of surgery-induced delirium superimposed on dementia. Read more.
- Genetic cases of amyotrophic lateral sclerosis and frontotemporal dementia are most frequently caused by hexanucleotide expansions in C9orf72, which encodes a predicted guanine exchange factor. Although repeat expansion has been established to generate toxic products, mRNAs encoding the C9ORF72 protein are also reduced in affected individuals. In the latest issue of Nature Neuroscience, Al La Spada, MD, PhD, tested how C9ORF72 protein levels affected repeat-mediated toxicity. Read that article here.
- Leonard White, PhD, contributed to a report that produced the highest-ever resolution view of a brain using magnetic resonance imaging, showing details at 25 micrometers--about one-fourth the width of a strand of hair. See images from his work, and read the article in the latest issue of Neuroimage.
- White will also be co-editing a special issue of Frontiers in Integrative Neuroscience that aims to build bridges (experimental or conceptual) between the neurosciences and the humanities. The issue is currently seeking abstracts in this area. Submit yours or read more here.
Stroke
- Intravenous recombinant tissue plasminogen activator (rtPA) is an important treatment for treating acute ischemic stroke, but data on its safety in patients with recent gastrointestinal malignancy or recent gastrointestinal bleeding are limited. Senior author Ying Xian, MD, PhD, and colleagues and colleagues at the Duke Clinical Research Institute examined data from more than 40,000 elderly stroke patients receiving this treatment. Their analysis did not find an increased risk for mortality or bleeding for patients with gastrointestinal malignancy or recent gastrointestinal bleeding. Read more.