Members of the Duke Neurology Department contributed to seventeen peer-reviewed research studies published this August. Members of the lab of Nicole Calakos, MD, PhD, discovered that a medication created to treat patients with HIV may help people with dystonia. New translational research provided the most accurate atlas of the mouse model to date and answered questions about late-onset Alzheimer’s disease. Other articles examined the experiences of people with Parkinsons during periods when they stop taking their medication, discussed a form of Alzheimer’s related dementia that strikes extremely elderly patients, and a pair of interactive “Clinical Reasoning” essays that test your clinical knowledge. Read the summaries below to learn more about each of these studies and find links to the original articles themselves.
Memory Disorders
- A team of researchers including senior author Shih-Hsiu “Jerry” Wang, MD, PhD, John Ervin, and Kim Johnson, MD has identified a new, distinct cause of Alzheimer’s-related dementia among the oldest old. Their study shows that a condition known as LATE-NC or limbic-predominant age‐related TDP‐43 encephalopathy neuropathological change was associated with hippocampal sclerosis and arteriolosclerosis in this population. Read their full study in Acta Neuropathologica.
Parkinson’s Disease and Movement Disorders
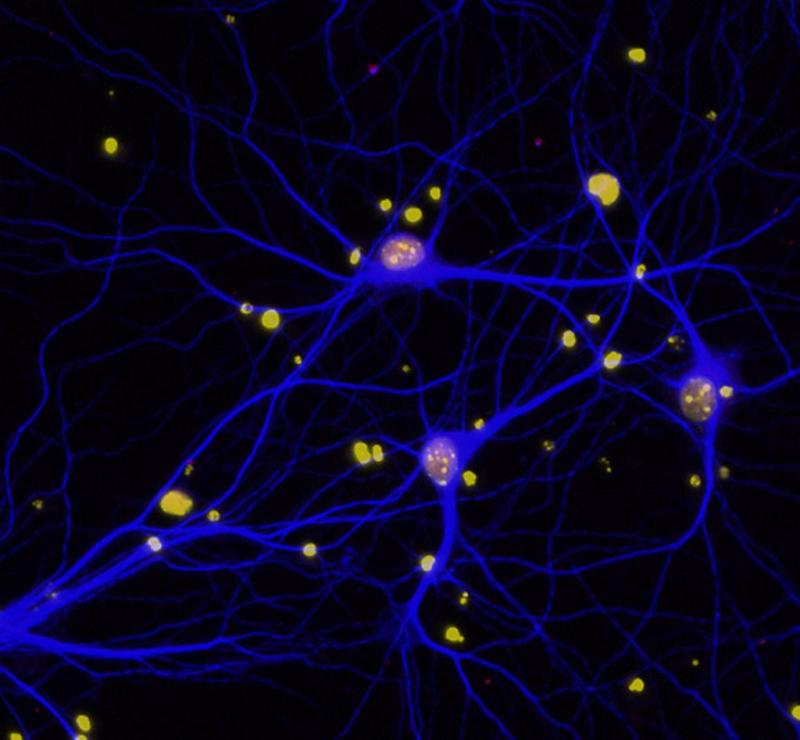
- Senior author Nicole Calakos, MD, PhD, Zachary Caffall, PhD, and Kunal Shroff identified a stress-dependent and nuclear compartment-specific proteome disruption caused by the dystonia-causing DYT-TOR1A genotype. Their study in Neurobiology of Disease opens a new research direction for DYT-TOR1A dystonia pathophysiology by shedding light on this vulnerability and its consequences for brain function. Read that study here.
- Nicole Calakos, MD, PhD, and Zachary Caffall, PhD, were also the senior authors of a new study that identified ritonavir, a HIV protease inhibitor as a potential disease-modifying therapy for dystonia. Miranda Shipman also contributed to the study, which was published in Science Translational Medicine. Read that article here.
- A new clinical reasoning interactive case report series by Burton Scott, MD, PhD, and recently graduated Duke Neurology resident Paul McIntosh, MD, discuss three patient cases involving movement disorders, including that of a 55-year-old man with odd behavior and abnormal movements. Read that case report inNeurology.
- Sneha Mantri, MD, MS, was the first author of a survey analyzing the lived experience of “off periods” (times without medication) for people with Parkinson's disease, including symptoms and coping strategies. The team identified the frequency of common symptoms experienced during these periods, triggers that lead to off periods, and coping mechanisms. Read that study in the Journal of Patient-Centric Research and Reviews.
- A new article in Parkinsonism and Related Disorders examined the frequency of suicidal ideation and associated clinical features in Lewy body dementia (LBD). A team including Kathryn Moore, MD, analyzed data from patients with LBD and symptoms of depression, finding that nearly one in five participants reported suicidal thoughts. The findings emphasize the importance of routine screening for psychiatric symptoms in LBD and intervention when such concerns are identified. Read the full article here.
General and Community Neurology
- Suma Shah, MD, and Ariel Lefland, MD, were the lead authors of a clinical reasoning case report series. The interactive series includes that of a 64-year-old man with multiple cranial neuropathies as well as hypertension, hyperlipidemia, and hypothyroidism. Read that article and answer questions about how to proceed in the latest issue of Neurology.
Neurocritical Care
- A new study shows promising results for CN-105, a novel therapy with the potential to reduce inflammation and speed recovery after stroke or brain injury. Senior authors Daniel Laskowitz, MD, MHS, and Michael “Luke” James, MD, examined 38 participants treated with CN-105 after intracerebral hemorrhage. Compared to matched cohorts, the participants had no higher rates of adverse reactions as well as lower 30-day modified Rankin Scale scores. Read the full article in Neurocritical Care.
Neuromuscular Disease
- Jeffrey Guptill, MD, MHS, and Yingkai Li, MD, PhD, were the lead authors of a new study that examined the effects of the autoantibody eculizumab (ECU) on the immune systems of individuals with myasthenia gravis. The team evaluated innate and adaptive immunity among patients before ECU and ≥3 months later while on stable therapy. Their findings extend our understanding of ECU's mechanism of action when treating patients with myasthenia gravis. Read the full article in Clinical Immunology.
- First author Shruti Raja, MD, and Jeffrey Guptill, MD, MHS, compared open versus minimally invasive thymectomy for patients with myasthenia gravis, finding lower odds of perioperative complications with for minimally invasive and transcervical surgeries compared to transthoracic surgeries. Read their article in the Annals of Thoracic Surgery.
Multiple Sclerosis and Neuroimmunology
- Identifying and quantifying treatment-emergent adverse events (TEAEs) is critical as new treatments for multiple sclerosis emerge. Bryan Walker, PA-C, MHS, was part of a team that analyzed patient reactions to cladribine tablets in two phase 3 clinical trials, finding the drug was well tolerated, with a low rate of TEAEs over the course of 12 weeks. Read that analysis in Multiple Sclerosis Journal - Experimental, Translational, and Clinical.
- In recent years, many fellowship programs focusing on multiple sclerosis and neuroimmunologic disorders have been created or expanded in academic medicine. Suma Shah, MD, was part of a workgroup that developed a consensus fellowship curriculum to guide current and future training programs and accreditation efforts. Read what that group discussed here.
- A new review by senior author Suma Shah, MD, and recent graduate Petra Brayo, MD examines available treatment strategies for patients with MOG-IgG associated disease for both the acute and long-term setting. Read that article in Current Treatment Options in Neurology.
Translational Brain Sciences
- While large multi-center genome-wide association studies (GWAS) have identified associations between numerous genomic loci and late-onset Alzheimer’s disease (LOAD), there remains a large, unmet need to for more precise data on the individual genes that cause disease, their specific variants, and the molecular mechanisms of action that lead to disease. Senior authors Ornit Chiba-Falek, PhD, and Julio Barrera conducted ATAC-seq profiling using NeuN sorted-nuclei from 40 frozen brain tissues to determine LOAD-specific changes in chromatin accessibility landscape in a cell-type specific manner. Read what they found in Molecular Neurodegeneration.
- Leonard White, PhD, led the development of a new multi-contrast, multidimensional atlas of the Wistar rat, which offers significant improvements over previous atlases. The new atlas should assist in our understanding of the complex anatomy of the rat brain and provide researchers worldwide a useful new platform for their work. Find that atlas and read about its development in the latest issue of NeuroImage.
- Even with antiretroviral therapy, up to half of people living with HIV will experience neurological or neurocognitive impairment. Simon Davis, PhD, contributed to a new article that advances our understanding of the types of impairment that occur. Along with colleagues at the Department of Psychiatry and Behavioral Sciences and Brain Imaging and Analysis Center, Davis examined white matter integrity in people living with HIV and identified cognitive impairment related to these structural and functional connectivity systems. This result clarifies the functional relevance of the corpus callosum in HIV and provides a framework in which abnormal brain function can be understood in the context of abnormal brain structure, which may both contribute to cognitive impairment. Read the full article in Human Brain Mapping.