This March, members of our Department contributed to studies that reveal potential new therapeutic targets for Alzheimer’s disease, help triage patients suffering from traumatic brain injury, address issues contributing to physician burnout, and more. In all, our faculty, staff, students, and trainees contributed to 15 studies published over the past 31 days. Read about them and find links to the original articles below.
Parkinson’s and Movement Disorders
- Spacing out physical therapy sessions appears to be a better approach to maintain physical function for people living with Parkinon’s disease, a new randomized clinical trial has found. A team including Kathryn Moore, MD, MSc, compared participants with Parkinson’s who received the same physical therapy sessions either twice a week or spaced out over six months, finding the physical abilities twice-weekly “burst” participants deteriorated compared to their counterparts receiving spaced out therapy. Read the full article in Parkinsonism & Related Disorders.
Neurocritical Care
- Clinicians often use prognostic calculators to predict outcomes for traumatic brain injury (TBI), but the outcomes measured are most relevant for severe TBI. Brad Kolls, MD, PhD, and colleagues at Duke Neurosurgery developed high performing machine learning models to predict trichotomized discharge disposition. These models can assist in optimization of patient triage and treatment, especially in cases of mild and moderate TBI. Read their analysis in Neurosurgery.
- A new study in JAMA Network Open provides insights into mortality and neurologic disability caused by intracerebral hemorrhage (ICH). The analysis of an ethnically and racially diverse cohort of more than 2500 patients found that larger log ICH, older age, presence of infection, and other factors were associated with higher mortality and disability at three months. Michael “Luke” James, MD, contributed to the study. Read it here.
Translational Brain Sciences
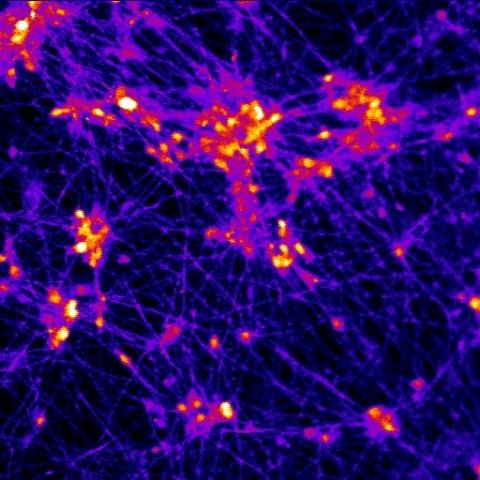
- A new study in Frontiers in Neuroscience advances our knowledge of the genetic factors contributing to depression onset in late-onset Alzheimer’s disease (LOAD) and the genetics underlying the heterogeneity of depression in LOAD. Senior authors Ornit Chiba-Falek, PhD, and Suraj Upadhya, as well as Michael Lutz, PhD, and colleagues developed a polygenic risk score for predicting depression in people living with Alzheimer’s disease. The developed polygenic risk score accurately predicted LOAD patients with depressive symptoms. Read the full article in Frontiers in Neuroscience.
- Michael Lutz, PhD, contributed to a new perspective article that discusses the relevance and advantages that Bayesian inference offers to clinical trials using the data from amyloid antibody aducanumab presented at a recent FDA hearing. Read that article in Alzheimer's & Dementia.
Stroke and Vascular Neurology
- A new study provides important insights into the clinical characteristics of COVID-19 in people with acute ischaemic stroke and identifies factors predicting functional outcome. A team including Andy Liu, MD, MS, and Simon Davis, PhD, found both a relationship between COVID-19-associated AIS and severe disability or death as well as factors such as elevated neutrophil-to-lymphocyte ratio, diabetes, and age >60 years were associated with worse outcomes. Read that article in the Journal of Neurology, Neurosurgery & Psychiatry.
- Brian Mac Grory, MB BCh, MRCP, and Deborah Rose, MD, were the senior authors of a case report discussing diagnostic and therapeutic considerations involving Down syndrome and moyamoya disease, especially in how both conditions affect the risk for stroke and cardiovascular disease. Child Neurology resident Lauren Chamberlain, DO, also contributed to the report, which appears in the British Medical Journal.
- Treating elevated low-density lipoprotein cholesterol (LDL-C) levels could be a helpful way to reduce risk of stroke, according to new research from a team including Daniel Laskowitz, MD, MHS, and Runqi Wangqin. The authors found that elevated LDL-C levels were associated with an increased risk for new ischemic stroke among patients without lipid-lowering treatment but not for patients receiving this treatment. Read that article in Stroke and Vascular Neurology.
- Brian Mac Grory, MB BCh, MRCP, was also part of a meta-analysis examining whether prolonged cardiac monitoring after stroke improved detection of atrial fibrillation not detected by conventional rhythm monitoring strategies, as well as stroke preventive strategies and stroke recurrence. The team’s analysis found that prolonged cardiac monitoring after an ischemic stroke or TIA can lead to higher rates of atrial fibrillation detection and anticoagulant initiation. However, it also found no solid evidence supporting that prolonged cardiac monitoring is associated with lower stroke recurrence risk. Read the full study in Neurology.
- Cranial electrical stimulation (CES) is a neuromodulation tool with promising but inconsistent results for epilepsy, depression, and other conditions. Wuwei “Wayne” Feng, MD, MS, and Pratik Chhatbar, MD were part of a new study that may sheds more light on this technique. The team directly measured the CES-induced voltage changes with implanted stereotactic-electroencephalographic (sEEG) electrodes in twenty-one epilepsy participants. They also examined the effects of stimulation frequency, intensity, electrode montage and age on electric fields in parts of participants. They found both measured voltages and electric fields obtained in vivo are highly correlated with the predicted ones in their cohort. Read the full study in Frontiers in Human Neuroscience.
Neurocritical Care
- Machine learning holds promise as a tool to guide clinical decision making by predicting in-hospital mortality for patients with traumatic brain injury, but there is room for improvement in existing models in developing and developed countries. Brad Kolls, MD, PhD, joined colleagues at Duke Neurosurgery to examine data from the Duke University Medical Center National Trauma Data Bank and Mulago National Referral Hospital in Uganda to predict in-hospital mortality for both settings. The team built six machine learning models for each data set and then selected the best model through nested cross-validation. Read the full study in Neurosurgery.
Memory Disorders
- Tuberous sclerosis complex (TSC) is an inherited neurodevelopmental disorder caused by mutations that causes a variety of neuropsychiatric symptoms. In a new research study, senior authors Andy Liu, MD, MS, and Jerry Shi-Hsiu Wang, MD, PhD, as well as James Burke, MD, PhD, John Ervin, Rich O’Brien, MD, PhD, and Jay Lusk examined whether the radiotracer flortaucipir is bound to phosphorylated tau in brains of patients with TSC and further sought to determine the specific tau isoform seen in TSC. Their findings could lead to a new era of anti-tau therapies used to treat both Alzheimer’s and TSC. Read the full study in Acta Neuropathologica Communications.
Other Topics
- Burnout in medicine, already a problem before COVID-19, has become a national crisis over the past two years, despite the additions of mindfulness meditation apps, lunchtime yoga classes, and other proposed solutions. Sneha Mantri, MD, MS, was the first author of a commentary that discusses how these solutions focus on individual factors rather than systemic changes. It also offers suggestions towards long-term improvement. Read that article here.
- First author Shruti Raja, MD, as well as Vern Juel, MD, contributed to the first-in-human clinical trial of NTM-1633, a novel mixture of monoclonal antibodies against botulinum toxin e. The trial found that NTM-1633 was well tolerated and had favorable safety, tolerability, pharmacokinetics, and immunogenicity. Read that article in Antimicrobial Agents and Chemotherapy.
- Shruti Raja, MD, also contributed to an article describing the first-in-human, phase 1 trial of DM1157 in healthy adult volunteers that was halted early because of significant toxicity. This study provides an important example of the risks and challenges of conducting early phase research as well as the role of modeling and simulation to optimize participant safety. Read it in Infectious Diseases and Therapy.