New research from the Duke Department of Neurology is advancing treatment of neurological conditions, uncovering secrets about how our brain and nervous system function, and refining training for the world’s next generation of neurologists. Highlights from February 2019 include a study identifying gender differences in sleep apnea, a new approach to identifying seizures in neuro-intensive care units, and studies examining the origins of ALS and other neurodegenerative disorders at the cellular level. Here are short summaries of these and other studies published in February 2019 by members of our Department.
Neurodegeneration and Neurotherapeutics
- Al La Spada, MD, PhD, and Somasish Dastidar, PhD, contributed to a study that examined how the FUS gene contributes to amyotrophic lateral sclerosis. The team found that overriding FUS autoregulation in mice led to growing toxicity in cells followed by ALS-like symptoms. Read the full results of their study in eLife here.
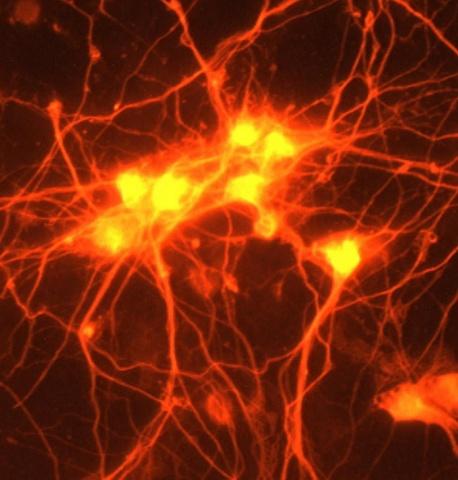
- La Spada was also part of a research team that investigated the role that astroglia, star-shaped cells found in the brain,played in the development of fragile X-associated tremor/ataxia syndrome (FXTAS) a late-onset neurodegenerative disorder. Read the results of their study in the latest issue of Acta Neuropathologica Communications here.
Epilepsy, Sleep, and Neurophysiology
- Men and women show different symptoms of obstructive sleep apnea (OSA), according to new research by senior author Andrew Spector, MD, former Duke Neurology fellows Damien Earl, MD, and Sushil Lakhani, MD, and Brigham and Women’s Hospital Daniel Loriaux, MD. A retrospective analysis of 545 subjects found that BMI, neck circumference, and sleepiness predicted OSA for men, while older age, neck circumference and morning headaches were predictive for women. Read that full study here.
- Non-convulsive seizures are a common complication within neurological intensive care units. Lead authors Christa Swisher, MD, and Jennifer Kang, MD, as well as Saurabh Sinha, MD, PhD, and G. Clay Sherill evaluated an innovative approach to detect these seizures more quickly: quantitative EEG (qEEG), which provides a time-compressed, simulated visual display from raw EEG data. The team found that nurses trained in qEEG were able to accurately detect seizures, with a sensitivity of 85.1% and a specificity of 89.9% compared to conventional EEG. Read that full study in Neurocritical Care.
Education
- Oral case-based assessments are an important part of the neurology residency experience, especially for neurological emergencies. Spector, Sinha, as well as former Duke neurology residents Aaron Loochtan, DO, and David Lerner, MD, evaluated six of these case-based assessments with a group of trainees and attendings. Their analysis both confirmed the value of these exams and identified area for improvement. Read their full article in the latest issue of Neurologist.