Faculty from the Duke Department of Neurology contributed to seven new peer-reviewed journal articles in January 2020. A team including Simon Davis, PhD, helped to answer questions about how the brain forms and stores memory. Christa Swisher, MD, Christian Hernandez, MD, and colleagues evaluated a promising new tool that offers improved in-patient seizure detection. Other stories this month offer a timeline about when it is safe to offer IV tPA to previous stroke patients, evaluate a new therapy for recurrent glioblastoma, answer new questions about the subcellular origins of breast cancer, among other topics.
Epilepsy
- The 2HELPS2B inpatient seizure risk prediction tool offers promise for improving inpatient seizure risk detection and improve continuous electroencephalogram (cEEG) cost-effectiveness. A team including Christa Swisher, MD, Christian Hernandez, MD, and medical student Safa Kaleem validated this tool in the latest issue of JAMA Neurology, analyzing clinical and EEG data from more than 2,000 patients from a variety of medical centers. Read that study here.
Neuro-Oncology
- Katy Peters, MD, PhD, was part of a team that evaluated the safety and efficacy of VB-111, an anti-cancer gene therapy, for patients with recurrent glioblastoma. Their phase I/II study of 72 patients found improved survival for patients and that VB-111 was well tolerated. Read their study in Neuro-Oncology.
Neurodegeneration and Neurotherapeutics
- Mammalian cells rely on autophagy to clear themselves of debris and to function over the long term. Building on previous research that found that ovarian cancer cells lose genes associated with autophagy, a team including Al La Spada, MD, PhD, found that reducing an autophagy gene in mice lead to earlier ovarian tumors, showing that ovarian carcinomas gain their hallmark genomic instability in part by losing autophagy genes. Read their PLOS Genetics story here.
Translational Brain Sciences
- Research has identified the presence of APOE4 alleles as the most important genetic risk factor for late-onset Alzheimer’s disease, but the specific impact of different APOE4 alleles on brain aging, by gender, and on other factors remains unclear. Lead author Alexandra Badea, PhD, Carol Colton, PhD, and colleagues identified vulnerable brain circuits in novel mouse models which had either human APOE3 or APOE4 gene alleles. Their analyses revealed not just genotype, but also sex specific differences. Read their article in Frontiers in Neuroinformatics.
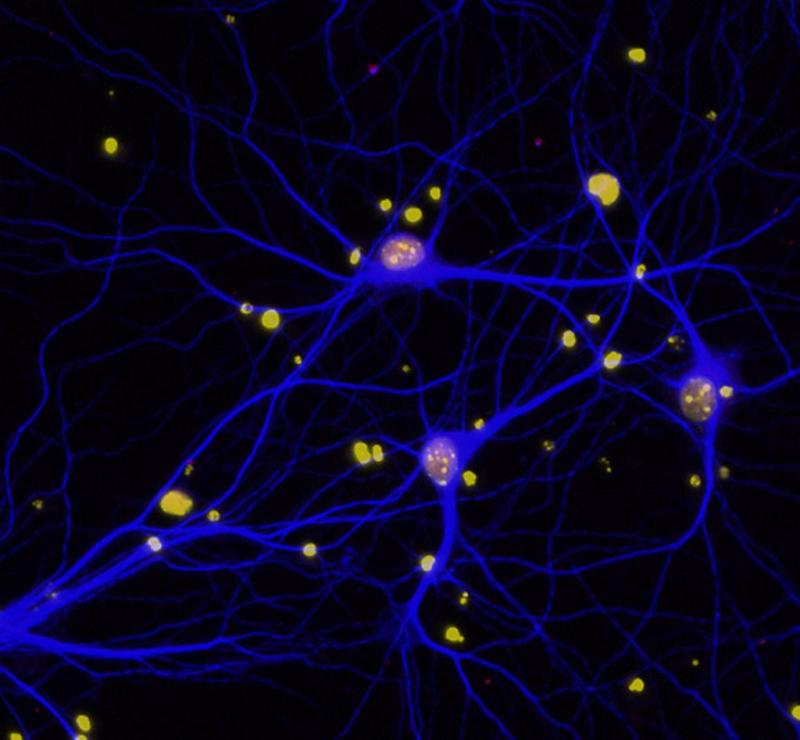
- Simon Davis, PhD, contributed to a study in the Journal of Neuroscience that examines how neural pattern similarity between repeated exemplars of a concept affects both true and false memories for target or lure images. They found that increased overlap in cortical representations for conceptually-related pictures is associated with increased accurate recognition of repeated concept pictures. Read their article here.
Stroke and Cardiovascular Disease
- Intravenous tissue-type plasminogen activator (IV tPA) only increases the risk for brain hemorrhage in patients with previous stroke if the prior occurred within the past two weeks, a new study has found. This retrospective observational study, by Shreyansh Shah, MD, Ying Xian, MD, PhD, and colleagues, appears in Circulation Cardiovascular Quality and Outcomes.
- Xian also contributed to a study assessing the predictive value of the Global Registry of Acute Coronary Events (GRACE) discharge score for patients with stable coronary artery disease (SCAD) after percutaneous coronary intervention (PCI). Their analysis of more than 4,000 patients with SCAD who underwent PCI found that the GRACE discharge score was an effective predictor for risk stratification of death and related risk factors. For this patient group. Read their study in Catheterization and Cardiovascular Interventions.