Members of the Duke Department of Neurology contributed to nine studies in peer-reviewed journals published in December 2019. In the fields of neurodegeneration and neuromuscular disease, our faculty found potential new avenues for therapies for spinocerebellar ataxia type 7 (SCA7) and myasthenia gravis. Other studies by our faculty and housestaff answered important questions about how reductions in blood pressure affect outcomes for thrombectomy, outcomes for deep brain stimulation for patients with Parkinson’s, and other areas. Read summaries about each of these articles, and find links to the original studies below.
Neurodegeneration and Neurotherapeutics
- New research sheds light on the origins of SCA7 and demonstrates effective new therapeutic pathways for SCA7 and the more than 40 other types of spinocerebellar ataxia. The study, which appears in Neuron, implicates metabolic dysregulation leading to altered calcium homeostasis in neurons as the underlying cause of cerebellar ataxias. Read it here.
- La Spada also contributed to a new statement from the American College of Medical Genetics and Genomics that examined whether there was sufficient evidence to support BRCA1/2 and other inherited breast cancer genetic testing for all breast cancer patients. Read that full statement in Genetics in Medicine.
Stroke
- Christa Swisher, MD, Shareena Rahman, MD, and Ovais Inamullah, MD, were part of a multicenter retrospective study that examined the associations between reductions in systolic blood pressure and mechanical thrombectomy. The analysis of nearly 1,400 patients found that reductions in systolic blood pressure were inversely associated with poor outcomes but not safety outcomes. Read the full article in the Journal of Neurointerventional Surgery.
Neuroimmunology
- Existing normative flow cytometry data have several limitations, such as small sample sizes, incompletely described study populations, variable methodology, and limited depth for defining lymphocyte subpopulations. Jeffrey Guptill, MD, MHS, was the senior author of a study that provides resources to better compare and extract data for subjects across gender, race, and age group. Read that study in PLoS One.
Neuromuscular Disease
- Therapies that target Th17 cells could be a fruitful avenue for helping patients with myasthenia gravis, according to a new study by senior author Jeff Guptill, MD, MHS, Karissa Gable, MD, Vern Juel, MD, Janice Massey, MD, Shruti Raja, MD, Lisa Hobson-Webb, MD, and Melissa Russo. The team found that the transcription factor RoRy, reduced the frequency of Th17 cells without affecting other T helper subsets. Read that article in Experimental Neurology.
General Neuroscience
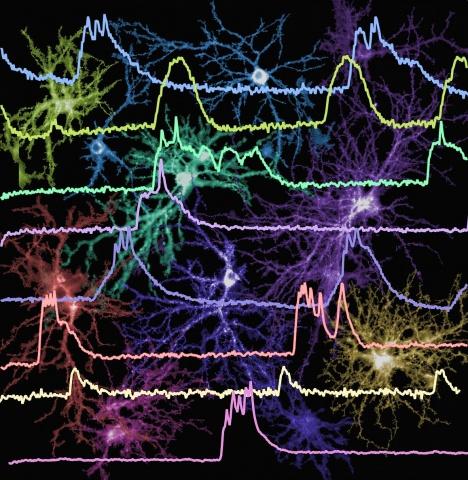
- Miguel Nicolelis, MD, PhD, was the senior author an analysis in Scientific Reports that examined the pitfalls and shortcomings of rotational dynamics, a proposed type of neuronal processing that exists in organisms from leeches to primates. Read that article here.
Movement Disorders
- Sneha Mantri, MD, MS, contributed to a nationwide analysis of readmission and post-operative outcomes for Parkinson’s patients who have had deep brain stimulation surgery. Their analysis of more than 6,000 patients found favorable short-term hospitalization rates after DBS as well as persistent socioeconomic disparities in DBS. Read the full study in Parkinsonism and Related Disorders here.
Memory Disorders
- Andy Liu, MD, was the first author of a JAMA Neurology study that answers important questions about the neuropsychiatric symptoms associated with tuberous sclerosis. Their case control study found that adults with tuberous sclerosis had similar cognitive and behavioral difficulties, as well as similar cerebrospinal fluid biomarkers, than patients with frontotemporal dementia. Read that study here.
Sleep Disorders
- Transvenous phrenic nerve stimulation (PNS) shows promise as a treatment for central sleep apnea, according to a study in the Journal of Clinical Sleep Medicine. Andrew Spector, MD, and colleagues examined nearly 200 patients who had received transvenous PNS, finding that it significantly improved CAS severity, sleep quality, ventricular function and quality of life, regardless of whether patients had heart failure. Read their full study here.