Just in time for National Stroke Month, members of the Duke Neurology Department contributed to three stroke-related research articles in May. These papers found surprising results about treatment patterns for younger stroke patients, paradoxical relationships between Hb A1C levels and stroke outcomes, and identified risk factors for stroke among individuals with peripheral artery disease (PAD). In addition, members of our faculty contributed to seven articles in other disciplines, uncovering new information about brain plasticity, pioneering new therapies for spinal cord injuries, and reviewing treatment options for myasthenia gravis. Read summaries of those stories and find links to the original articles below.
Neuromuscular Disease
- The latest issue of Clinical Neurophysiology featured an international consensus statement on the current status of Single Fiber EMG (SFEMG) and the measurement of neuromuscular jitter with concentric needle electrodes (CNE – CN-jitter). Don Sanders, MD, was one of the primary editors of these new International Federation of Clinical Neurophysiology guidelines, which are available here.
- For the vast majority of patients myasthenia gravis, antibodies are responsible for the disruption of effective neuromuscular transmission. Senior author Vern Juel, MD, and Duke Neurology alumnus Amanda Guidon, MD, wrote an editorial for Neurology that discusses the use of efgartigimod as a novel antibody depletion therapy for this condition. Read that editorial here.
- Different brands of branded intravenous immunoglobulin (IVIG) treatment exist for patients with chronic inflammatory demyelinating polyneuropathy (CIDP). These brands vary in their production process, formulation, and other qualities Jeffrey Guptill, MD, MHS, was the first author of a study that examined two retrospective databases to look for patterns when patients switched these medications. Read what they found in Patient Preference and Adherence.
General Neurology/Neuroscience
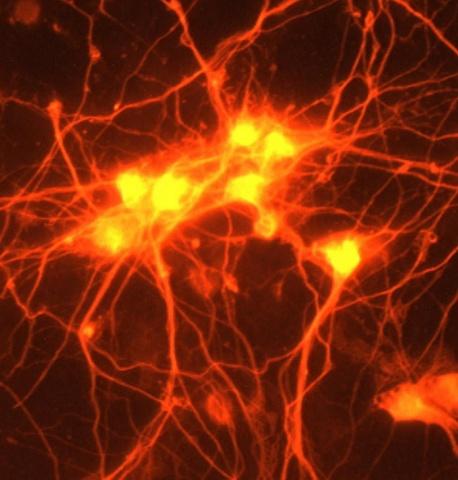
- The brain’s underlying plasticity, or ability to adapt in response to the environment is an important concept, but how this change actually happens has not been well documented. Senior authors Rich O’Brien, MD, PhD, and Alexandra Badea, PhD, used magnetic resonance imaging (MRI) in live mice to detect how their brains changed, following up with additional imaging after the mice died. Their findings may be useful in future efforts to improve rehabilitation and recovery after brain injury. Read their study in PLoS One.
- While surgery is typically the best medical treatment for pituitary tumors, questions remain about how this surgery affects patients quality of life after surgery. A team including Casey Farin, MD, surveyed 23 patients about their symptoms and quality of life before and after surgery to remove their tumors. They found significant short-term improvements in fatigue, numbness, memory, and other factors, as well as some reductions in sleep quality. Read their full study here.
Neurorehabilitation
- Senior author Miguel Nicolelis, PhD, and colleagues pioneered a neurorehabilitation setup for patients with spinal cord injuries. Their setup combined several approaches that have already been found to help patients with these injuries. Patients were able to walk with partial body support, and showed improved cardiovascular fitness and even some neurological recovery. Read the full article in Scientific Reports.
Stroke
- Younger stroke patients represent an important, often overlooked population. First author Jodi Dodds, MD, Ying Xian, MD, PhD, and colleagues at the DCRI examined data from more than 30,000 patients who had a stroke to find out whether they were receiving tPa, and if they were receiving prompt treatment. Read what their surprising results in the latest issue of Neurology.
- Xian also contributed to a DCRI study that uncovered a paradoxical relationship between hemoglobin A1C and in-hospital mortality among patients with intracerebral hemorrhage. The team found that both high and low levels of Hb A1C were associated with higher mortality and worse outcomes. Read more about their findings in Heliyon.
- The risk factors for stroke among patients with peripheral artery disease (PAD) are poorly understood. Using data from the EUCLID study, lead author Brad Kolls, MD, PhD, MCCI, and colleagues, identified several independent risk factors for stroke among this group, including age, prior stroke, prior atrial fibrillation/flutter, diabetes mellitus, higher blood pressure, prior amputation, lower ankle-brachial index, and geographic region. They also found that ticagrelor, compared to clopidogrel, appeared to reduce the chance of future stroke. Read the full study in Stroke here.
Memory Disorders
- Building on previous research that observed that protein interacting with amyloid precursor protein (APP) tail 1 (PAT1), is poorly associated with APP at the cell surface of primary neurons, a team including Lidia Tagliafierro, PhD, found that PAT1 is involved in early endocytosis. Read that article in Cellular and Molecular Life Sciences.