This October, members of the Duke Neurology Department contributed to 11 new peer-reviewed journal articles, advancing the fields of clinical and translational neuroscience. Highlights from the past 31 days include descriptions of a new technology that uses retinal scans to detect mild cognitive impairment, a white paper outlining challenges and opportunities for clinical trials in Alzheimer's disease, and genetic analyses that advance our understanding of the origins of Alzheimer’s disease. Read the paragraphs below for brief summaries of these and other articles as well as links to the original research articles themselves.
Epilepsy, Sleep, and Clinical Neurophysiology
- Shruti Agashe, MD, was the first author on a paper that provided a comprehensive review of intracranial hemorrhage in sEEG regardless of clinical symptoms. She also identified electrographic correlates of hemorrhage to help in early detection. Read that article in the Journal of Clinical Neurophysiology.
General and Community Neurology
- Leonard White, PhD, was the senior author of a new study detailing an improved rapid workflow for neuron counting in combined light sheet microscopy and magnetic resonance histology. This workflow improves the accuracy of neuron counting and the assessment of neuronal density on a region-by-region basis, with broad applications for studies of how genetics, environment, and development across the lifespan impact cell numbers in the central nervous system. Read more about this workflow in Frontiers in Neuroscience.
Memory Disorders
- A new diagnostic technology is able to use retinal scans to distinguish between people with mild cognitive impairment (MCI) and normal cognition, thanks to a collaboration between the Duke Departments of Ophthalmology. Senior author Sharon Fekrat, MD, Andrew Liu, MD, MS, Kim Johnson, MD, and colleagues developed a multimodal convolutional neural network (CNN) that examined multimodal convolutional neural network (CNN), and compared retinal images from cognitively normal subjects and those with MCI. Read that article in Ophthalmology Science.
- Effective, accurate clinical trials are needed to develop new therapies for Alzheimer’s disease, but the slow, varied progression of this condition makes these trials difficult. Kathleen Welsh-Bohmer, PhD, was the first author of a new article that addresses these challenges as well as new directions and actionable steps to improve future trial designs. Read that article in Alzheimer’s & Dementia.
Multiple Sclerosis and Neuroimmunology
- Catatonia is a complex, life-threatening neuropsychiatric syndrome that can possibly develop from autoimmune encephalitis. To aid in the diagnosis of this condition, a group including Mark Skeen, MD, created a video-based case report documenting one woman’s cataonia, which was ultimately determined to be secondary to anti-N-methyl-d-aspartate receptor encephalitis. View that case report in the Primary Care Companion for CNS Disorders.
Stroke and Vascular Neurology
- Brian Mac Grory, MB Bch, MRCP, contributed to a new analysis of the performance of thrombectomy-capable stroke centers (TSCs), a recently introduced intermediate tier of accreditation for hospitals where patients with acute ischemic stroke receive care. The team examined data from nearly 50,000 patients who received endovascular thrombectomy (EVT) and intravenous thrombolysis reperfusion therapies, comparing the quality of cares at TSCs to that at primary stroke centers (PSCs), and comprehensive stroke centers (CSCs). They found that CSCs and TSCs exceeded PSCs in key quality-of-care reperfusion metrics and outcomes. Read their article in Circulation.
- Brian Mac Grory, MB BCh, MRCP, and Ying Xian, MD, PhD, replied to a recent commentary article in JAMA discussing their research on vitamin K antagonists and intracranial hemorrhage after endovascular thrombectomy. Read that article here.
Translational Brain Science
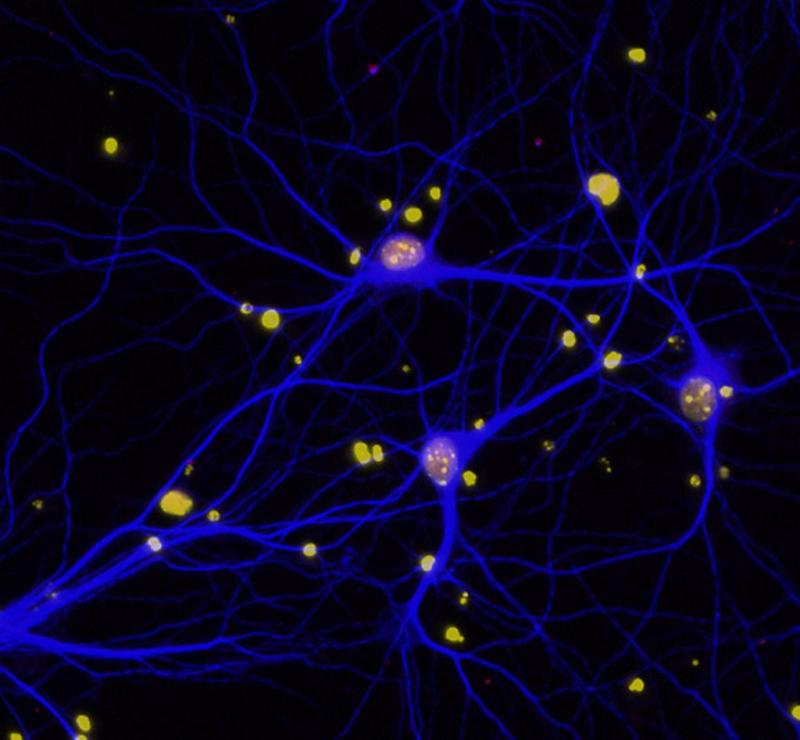
- Although numerous loci associated with late-onset Alzheimer’s disease (LOAD) have been discovered, the causal variants and their target genes remain largely unknown. To answer this question, senior author Ornit Chiba Falek, PhD, Daniel Gingerich, MS, E. Keats Shwab, Cordelia Hume, and colleagues performed the largest parallel single-nucleus multi-omics study to simultaneously profile gene expression and chromatin accessibility to date, using nuclei from 12 normal and 12 LOAD brains. Their analysis suggests that cell subtype-specific cis–trans interactions between regulatory elements and TFs, and the genes dysregulated by these networks contribute to the development of LOAD. Read their full study in Cell & Bioscience.
- Laurie Sanders, PhD, was part of a team that developed a CRISPR interference (CRISPRi) system based on the nuclease dead S. aureus Cas9 (SadCas9) fused with the transcriptional repressor domain Krueppel-associated box to controllably repress alpha-synuclein expression at the transcriptional level. Their approach presents a new model to understand safe levels of alpha-synuclein downregulation and a novel therapeutic strategy for PD and related alpha-synucleinopathies. Read more about it in Scientific Reports.
- Alexandra Badea, PhD, contributed to a study that developed an imaging-based pipeline to comprehensively assess cardiac structure and function in mouse models expressing different APOE genotypes using photon-counting computed tomography. Their team found results that PCCT offered high-quality imaging with reduced noise, demonstrating potential for the technique. Read more about their work in PLoS One.
Other
- Suma Shah, MD, was part of a randomized controlled trial investigating the effects of cryocompression therapy on chemotherapy-induced peripheral neuropathy. Shah and colleagues enrolled 91 gynecologic cancer patients planned for five to six cycles neurotoxic chemotherapy and assigned them to receive cryocompression on their dominant hand or foot, and no cryocompression on the opposite limb. The therapy decreased the odds of patients’ sensory neuropathy by 46% at their final visit. Read the full article in Obstetrics & Gynecology.