This September, members of the Duke Neurology Department contributed to 26 new studies, advancing our knowledge of neuroscience at the subcellular, national, and global levels. Ornit Chiba-Falek, PhD, and Laurie Sanders, PhD, lead studies that answered questions about the genetic origins of Parkinson’s disease and its connection to some forms of breast cancer. Meanwhile, Ying Xian, MD, PhD, and Shreyansh Shah, MD, and colleagues at the Duke Clinical Research Institute examined data from more than 250,000 stroke patients to examine how treatments of stroke differ depending on whether that stroke occurs inside or outside of a hospital. And Deborah Koltai, PhD, was an author and editor of 11 articles in a special issue of Epilepsy and Behavior providing a comprehensive analysis of the cultural, medical, and economic factors affecting epilepsy care in Uganda. Read more about these studies and more, and find links to the original articles, in the paragraphs below.
Neurocritical Care
- To date, there remains a lack of high-quality data on how to best define, document, and respond to brain death/death by neurologic criteria (BD/DNC). As part of the World Brain Death Project, an international panel of experts including Cherylee Chang, MD, worked together to analyze literature on this subject and provided minimum clinical criteria to determine BD/DNC. Read that article in JAMA.
- A new article in the latest issue of Neurocritical Care examined the neuroprotective potential of argon inhalation in traumatic brain injury in vivo in a group of mice. Daniel Laskowitz, MD, MHS, Haichen Wang, MD, and Viviana Cantillana contributed to the study, which is available here. Read more.
General and Community Neurology
- Andrew Spector, MD, co-wrote a letter to the editors of The Journal of Allergy and Clinical Immunology: In Practice discussing opportunities to enhance the AAAAI Physician Burnout Survey. Read that letter here.
Epilepsy, Sleep and Neurophysiology
- Status epilepticus remains a neurologic emergency with high morbidity and mortality, and there are many unanswered questions about optimal early treatment. Vishal Mandge, MD, and Aatif Husain, MD, wrote a review article in the Journal of Clinical Neurophysiology that describes important drug trials that have shaped our understanding of the treatment of status epilepticus and proposes clinical trial methodology considerations for all stages of the condition. Read that article here.
- Epilepsy is the most common serious chronic neurological disease in the world. Treating this condition in developing countries requires considering a host of concerns, including local cultures and belief systems about epilepsy, lack of access to medicine, patterns of health care use, and resources available in local hospitals. Deborah Koltai, PhD, was the guest editor of a recent issue of Epilepsy and Behavior that examine how culture, resources, and disease intersect with epilepsy care in Uganda. The 11 articles in this issue include discussions of opportunities and future directions from studying the cultural context of epilepsy care, how stakeholders and healthcare providers view barriers to care, and a systematized literature review of stigma interventions for epilepsy. Read those articles and more here.
- Non-invasive positive pressure ventilation (NPPV) is a technique used to deliver mechanical ventilation to patients with respiratory failure through a noninvasive interface such as nasal mask, facemask, or nasal plugs. In the latest issue of Chest, Andrew Spector, MD, and former sleep fellow Shravana Deepthi Gudivada MD, discuss how they qualify inpatients with acute on chronic hypercapnic respiratory failure for home NPPV at the time of discharge. Read their article here.
Memory Disorders
- Brenda Plassman, PhD, was the co-author of a Neurology article that examined interactions between sex, race, and risk of dementia diagnosis after traumatic brain injury among older veterans. Their analysis of a large, nationwide cohort found an increased risk for all races with the highest risk of dementia following TBI for white veterans. Read that article here.
- A new study in the Journal of Alzheimer’s Disease, helped answer questions about how aerobic exercise and a healthy diet improve neurocognition. A team including James Burke, MD, PhD, and Kathleen Welsh Bohmer, PhD, examined the associations between changes in metabolic, neurotrophic, and inflammatory biomarkers with executive functioning among participants in a trial of older adults with cognitive impairment randomized to receive a healthy diet, exercise, both, or a control condition. They found several metabolic biomarkers associated with increases in executive function. Read that study here.
Neurodegeneration and Neurotherapeutics
- Genetic studies have identified variants in the LRRK2 gene as important components of the pathobiology of Parkinson’s disease. The Duke Center for Neurobiology and Neurotherapeutics’ Andrew West, PhD, was the senior author of a new article discussing the biomarker regulatory process for Parkinson’s disease, emerging LRRK2 biomarker candidates, assays, underlying biomarker biology, and clinical integration. Read that article in Frontiers in Neuroscience.
Translational Brain Sciences
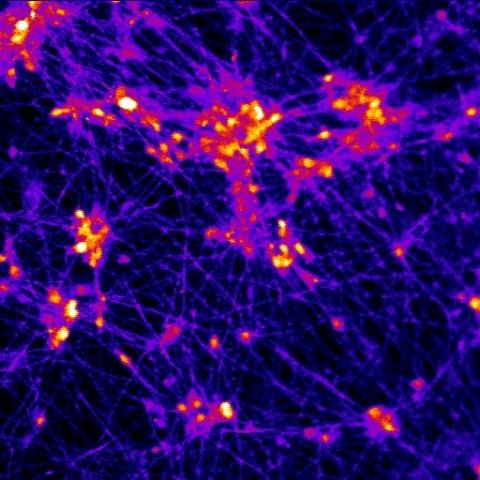
- Alpha-synuclein SNCA appears to play a role in the origins of Parkinson's disease (PD); however, the normal function of this protein and the pathway that mediates its pathogenic effect has yet to be discovered. Ornit Chiba-Falek, PhD, was the senior author of a new study investigated the mechanistic role of SNCA in the nucleus utilizing isogenic human-induced pluripotent stem cells-derived neurons from PD patients with autosomal dominant mutations, A53T and SNCA-triplication, and their corresponding corrected lines by genome- and epigenome-editing. Read that article in Human Molecular Genetics.
- Simon Davis, PhD, was the lead author of a new Cerebral Cortex study that used functional magnetic resonance imaging (fMRI) and representational similarity analysis to examine how visual and semantic representations predicted subsequent memory for single item encoding. Read that study here.
- The TRPV-4 ion channel helps regulate the blood-brain barrier, making it a potential therapeutic target for efforts to reduce neuroinflammation associated with dysfunction of the blood-brain barrier. A team including Wolfgang Liedtke, MD, PhD, investigated the role the ion channel plays in permeability of the blood-brain barrier during periods of neuroinflammation. Read what they found in Frontiers in Cell and Developmental Biology.
- Diseases of the central nervous system have historically been among the most difficult to treat using conventional pharmacological approaches. Viral-mediated gene transfer represents an attractive alternative for the delivery of therapeutic cargo to the nervous system. Ornit Chiba-Falek, PhD, contributed to a review article discussing the potential of this technique for new strategies for treating neurodegenerative disease. Read that article in Frontiers in Molecular Neuroscience.
- A new study in the American Journal of Pathology found that the mutation that causes the most common type of familial Parkinson’s disease also appears to directly increase the risk for breast cancer. Senior author Laurie Sanders, PhD, postdoctoral associate Claudia Gonzalez -Hunt, PhD, and colleagues found that somatic LRRK2 mutations, the most common cause of familial Parkinson’s disease occur frequently in breast cancer. The high mutation burden seen in this subset of tumors suggest that LRRK2 mutations may herald benefit from immune checkpoint inhibition. Read that study here.
Parkinson’s and Movement Disorders
- The FDA approved the use of levodopa oral dry powder inhalation for Parkinson’s patients whose current carbidopa/levodopa dose is wearing off prematurely. But this treatments not recommended for patients with chronic respiratory diseases, such as asthma and/or chronic obstructive lung disease (COPD). A team including Jeffrey Cooney, MD, discuss the existing evidence and recommendations for this subset of patients. Read that discussion in Parkinsonism & Related Disorders.
- Resident Amanda Currie, MD, contributed to a new pilot study that examined subthalamic nucleus (STN) deep brain stimulation on outcomes for patients with Parkinson’s disease. The Neurology article found that STN DBS reduced the odds of requiring polypharmacy and reduced the likelihood of tremor at five years. Read that article here.
Stroke
- Even though many acute ischemic strokes occur while patients are hospitalized, there are limited data on the rates of intravenous thrombolysis or endovascular therapy for patients who experience a stroke while in a hospital. Ying Xian, MD, PhD, and Shreyansh Shah, MD contributed to a JAMA Neurology study that compared data from more than 250,000 patients who underwent reperfusion therapy for stroke either in or out of a hospital. Among other findings, they found that in-hospital stroke onset was associated with reperfusion therapy, longer delays to reperfusion, and worse functional outcomes. Read that article here.