
The procedure involves implanting electrodes into the brain, which are then connected to a small pulse generator which is placed just under the skin in the chest. The pulse generator delivers electrical impulses to the brain that modify abnormal brain activity, reducing tremors, stiffness, and other symptoms.
But DBS devices have relied on a “one size fits all” approach, sending signals at a constant, steady rate, regardless of the individual patient needs or how the symptoms and severity of disease fluctuates over time. An interdisciplinary team of neurologists, neurosurgeons, and biomedical engineers at Duke is working to improve that model.
“No two brains are alike, and neither are any two cases of movement disorders,” said Kyle Mitchell, MD, a Duke neurologist who monitors and programs DBS at the Duke Movement Disorders Clinic. “Everyone’s brain anatomy is a little different, symptoms vary in their type and severity, and people have different responses to medications. We’d love to be able to personalize our DBS to meet every individual patient’s needs.”
At Duke, efforts to personalize and improve DBS are proceeding along two fronts. Warren Grill, PhD, Professor of Biomedical Engineering, is developing new software for DBS that could improve the signals DBS provides to the brain. “If you listen to the cells in the brain, they fire in patterns, like the dots and dashes of morse code,” Grill said. “Yet the stimulation DBS has done so far has been all dots.”
Grill has developed DBS software that returns the equivalent of both dots and dashes to the brain in computer and animal models. Preliminary results in persons with Parkinson’s disease indicate great improvements in the devices’ ability to reduce symptoms and improve quality of life for Parkinson’s.
Engineering New Technologies to Improve Clinical Care
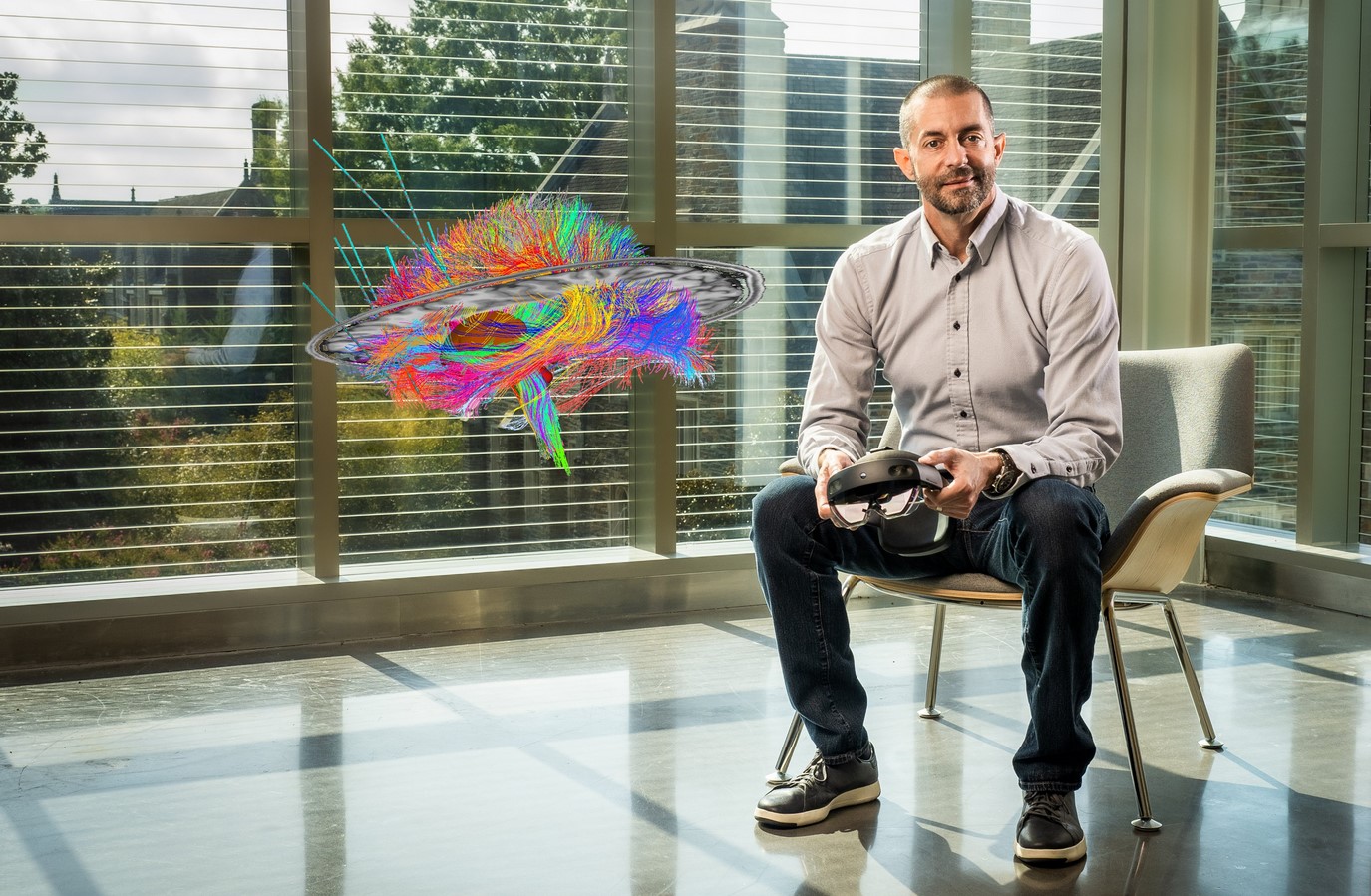
Cameron McIntyre, PhD, recently joined the team of neural engineers and scientists at Duke working to advance the existing technologies behind deep brain stimulation (DBS). A biomedical engineer with more than 20 years of research experience in neuromodulation, McIntyre has already developed numerous DBS technologies and is focused on solutions for improving the placement accuracy of the implanted electrodes.
“I'm really interested in working on how to bring together the best preoperative MRI data, with the best surgical planning models, to the next generation of neurosurgical robots,” he says. The research projects involve using reverse-engineering to refine the existing DBS software for the robotic stereotactic assistance device used in DBS surgery. “This work has the potential to improve DBS electrode placement and programming and help clinicians optimize the therapy for each patient,” he says.
McIntyre is also working on developing holographic clinical education materials for the DBS community, which would enable participants to visualize and interact with the models. “There is a substantial appetite for scientific education content around DBS,” he says. “This would be a powerful tool to help clinicians around the world understand the fundamental biophysics of how these devices actually work in the brain.”
With so many resources dedicated to improving DBS placement, targeting, and programming, the Duke team is keen on making technological advances that can rapidly reach clinical applications. “It’s not common to have so many neurosurgery, neurology, and engineering collaborators working together at one institution, and we are all striving to get new technologies into clinical practice in our lifetime,” says McIntyre.
A second parallel approach is being pioneered by Duke Neurosurgeon Dennis Turner, MD. Turner has developed an experimental “closed loop” DBS that can listen to the signals it receives from the brain and provide a tailored response. “An analogy for closed loop DBS is a smart thermostat,” Grill said. “If a furnace ran at the same rate regardless of the temperature outside, some days would be too cold or some days would be too hot. A closed loop DBS measures the electrical activity in the brain and adjusts stimulation accordingly.”
Grill hopes that future DBS devices take advantage of both innovations, allowing an improved DBS that provides optimal stimulation patterns in response to the individual needs and activities of the patient. “We’re fortunate to have experts in neurology, neurosurgery, and engineering working literally across the street from each other. This could open whole new pathways in personalized medicine,” he said.