About Us
The Chen Lab mainly studies sensory neurobiology of pain and itch, with a focus on TRP ion channels and neural circuits. The main objective of our lab is to identify molecular and cellular mechanisms underlying chronic pain and chronic-disease associated itch, using a combination of animal behavioral, genetic, molecular and cellular, advanced imaging, viral, and optogenetic approaches.
Research
There are three main research areas in the lab: Craniofacial pain, arthritis pain and joint function, and systemic-disease associated itch.
Craniofacial pain
Temporomandibular disorders (TMJD) include a group of painful conditions that involve the temporomandibular joint (TMJ), the muscles of mastication, and adjacent anatomic structures. In an effort to overcome limitations imposed by shortcomings in pre-clinical pain models of these disorders, we have reverse-translated measurements of bite-force, as a surrogate metric of TMJD pain, from human clinical research to the laboratory mouse (Pain. 2013, 154:1295-304). This approach is instrumental in defining the significant role of TRP ion channels in TMJD pain.
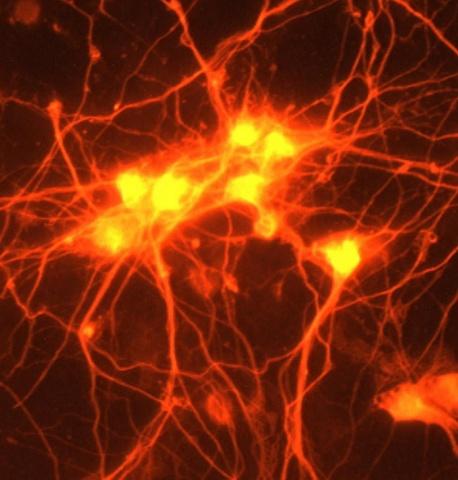
Human subjects with craniofacial pain conditions show greater levels of affective distress, environmental stress, somatic symptoms and pain catastrophizing compared with pain-free controls. The emotional toll of craniofacial pain, including TMJD, was higher than that of body pain. Using a novel activity-dependent technology “capturing activated neuronal ensembles” (CANE), we, together with a senior PI-Dr. Fan Wang’s group at Duke-Neurobiology, identified a hitherto unknown monosynaptic connection specifically between trigeminal ganglion (TG) sensory neurons and the lateral parabrachial nucleus-nociceptive neurons, which might provide a neural substrate for heightened craniofacial affective pain (Nat Neurosci. 2017, 20:1734-1743). Currently we are investigating how this monosynaptic connection would affect emotional aspects of craniofacial pain.
Arthritis pain and joint function
Chronic pain caused by arthritis affects millions of people in the US every year. About 25% of adults with arthritis report experiencing severe joint pain related to arthritis. Using behavioral, genetic, and tissue pathological analysis approaches, we have previously delineated an important role of TRPV1 in arthritis pain (Exp Neurol. 2009, 220:383-90; Osteoarthritis Cartilage. 2009, 17:244-51). Collaborating with a variety of groups, we have also identified the mechanosensitive Piezo-1 and -2 ion channels, both expressed in articular cartilage, are critical for the mechanotransduction of chondrocyte in response to injurious mechanical stress (PNAS. 2014, 111:E5114-22).
Psoriatic arthritis is a form of arthritis that affects a significant percentage of people who have psoriasis-a condition that features red patches of skin topped with silvery scales. Most people develop psoriasis first and are later diagnosed with psoriatic arthritis. Joint pain, stiffness and swelling are the main signs and symptoms of psoriatic arthritis. We are interested in determining the underlying mechanisms of psoriatic arthritis pain.
Systemic-disease associated itch
Treatment for itch (pruritus) associated with systemic disorders represents a severe unmet medical need for patients with cholestatic liver disease, chronic kidney disease, psoriasis, and some forms of lymphoproliferative disorders. Therapeutic recourse is dire because the underlying pathophysiology has remained largely elusive.
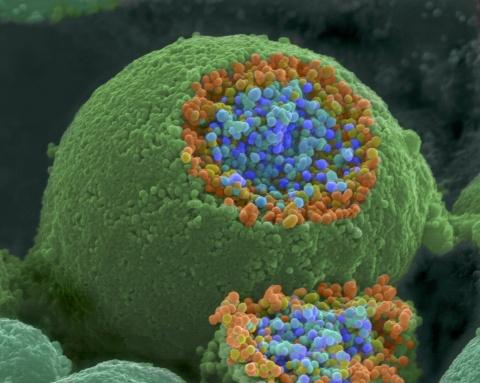
TRP ion channels have been implicated in the molecular mechanisms of peripheral sensory transduction of itch, with experimental studies supporting significant roles for the chemo-irritant receptor TRPA1 and the heat-capsaicin receptor TRPV1 in primary sensory neurons. TRPV4, a widely expressed multimodally-activated channel expressed in both innervated epithelia and sensory neurons, has also been found relevant for experimental itch. Our lab has demonstrated a novel pro-pruritic role of TRPV4 in skin keratinocytes using keratinocyte-specific Trpv4 knockout (KO) animals (J Biol Chem. 2016, 291:10252-62.). We are interested in examining whether and how keratinocyte-TRPV4 contributes to chronic disease-associated itch.
Our Team
Alumni
Michael Kim
PhD student (Duke Pathology)
Yuhui Luo, PhD
Visiting Scholar
PhD: Huazhong University of Science and Technology, China
Peng Wang
Research Technician
Abbie Suttle
Research Technician
Sabrina Takemoto-Spraggins
Undergraduate Student, Duke University, Class of 2025
Lauren Simmons
Undergraduate student, Biology, Class of 2023
Gwendolyn Henry
Undergraduate student, Psychology, Class of 2022
Publications
* denotes corresponding author
Dias FC, Wang ZL, Scapellato G, Chen Y*. Silencing of TRPV4-expressing sensory neurons attenuates temporomandibular disorders pain. Molecular Pain. 2023 doi: 10.1177/17448069231185696.
Wang P, Zhang QJ, Dias FC, Suttle A, Dong XZ, Chen Y*. TMEM100, a regulator of TRPV1-TRPA1 interaction, contributes to temporomandibular disorder pain. Frontiers in Molecular Neuroscience. 2023. 16:1160206
Suttle S, Wang P, Dias F, Zhang QJ, Luo YH, Simmons L, Bortsov A, Tchivileva IE, Nackley A, Chen Y*. Sensory neuron-TRPV4 modulates temporomandibular disorder pain via CGRP in mice. Journal of Pain. 2023. 24: 782-795
Zhang Y, Liang PF, Yang LH, Shan KZ, Feng LP, Chen Y, Liedtke, W, Coyne CB, and Yang HH. Functional coupling between TRPV4 channel and TMEM16F modulates human trophoblast fusion. Elife. 2022 Jun 7;11:e78840. doi: 10.7554/eLife.78840.
Yeo M#,*, Chen Y#,*, Jiang C, Chen G, Wang K, Chandra S, Bortsov A, Lioudyno M, Zeng Q, Wang P, Wang Z, Busciglio J, Ji RR*, Liedtke W*. Repurposing cell growth-regulating compounds identifies kenpaullone which ameliorates pathologic pain via normalization of inhibitory neurotransmission. Nature Communications. 2021 (#: co-first author; *: corresponding author)
Luo X, Chen O, Wang Z, Bang S, Ji J, Lee SH, Huh Y, Furutani K, He Q, Tao X, Ko MC, Bortsov A, Donnelly CR, Chen Y, Nackley A, Berta T, Ji RR. IL-23/IL-17A/TRPV1 axis produces mechanical pain via macrophage-sensory neuron crosstalk in female mice. Neuron. 2021. 109(17):2691-2706
Zhang Q, Henry G, Chen Y*. Emerging Role of Transient Receptor Potential Vanilloid 4 (TRPV4) Ion Channel in Acute and Chronic Itch. International Journal of Molecular Sciences. 2021. 22(14): 7591.
Chen Y*, Wang ZL, Yeo M, Zhang QJ, López-Romero AE, Ding HP, Zhang X, Zeng Q, Morales-Lázaro SL, Moore C, Jin YA, Yang HH, Morstein J, Bortsov A, Krawczyk M, Lammert F, Abdelmalek M, Diehl AM, Milkiewicz P, Kremer AE, Zhang JY, Nackley A, Reeves TE, Ko MC, Ji RR, Rosenbaum T, Liedtke W*. Epithelia-sensory neuron crosstalk underlies cholestatic itch induced by lysophosphatidylcholine. Gastroenterology. 2021 Apr 2:S0016-5085(21)00576-X. doi: 10.1053/j.gastro.2021.03.049.
Lee W, Nims RJ, Savadipour A, Zhang QJ, Leddy HA, Liu F, McNulty AL, Chen Y, Guilak F, Liedtke W. Inflammatory signaling sensitizes Piezo1 mechanotransduction in articular chondrocytes as a pathogenic feed-forward mechanism in osteoarthritis. Proceedings of the National Academy of Sciences. 2021 Mar 30;118(13):e2001611118
Luo Y, Suttle A, Zhang QJ, Wang P, Chen Y*. Transient Receptor Potential (TRP) Ion Channels in Orofacial Pain. Molecular Neurobiology. 2021 Jan 29. doi: 10.1007/s12035-021-02284-2.
Hua T, Chen B, Lu DY, Sakurai K, Zhao SL, Han BX, Kim JW, Yin LP, Chen Y, Lu JH, Wang F. General Anesthetics Activate a Potent Central Pain-Suppression Circuit in the Amygdala. Nature Neuroscience. 2020. 23(7): 854-868
Xu B, Zhang M, Shi X, Zhang R, Chen D, Chen Y, Wang Z, Qiu Y, Zhang T, Xu K, Zhang X, Liedtke W, Wang R, Fang Q. The multifunctional peptide DN-9 produced peripherally acting antinociception in inflammatory and neuropathic pain via μ- and κ-opioid receptors. British Journal of Pharmacology. 2020. 177(1):93-109
Zhang T, Zhang N, Zhang R, Zhao W, Chen Y, Wang Z, Xu B, Zhang M, Shi X, Zhang Q, Guo Y, Xiao J, Chen D, Fang Q. Preemptive intrathecal administration of endomorphins relieves inflammatory pain in male mice via inhibition of p38 MAPK signaling and regulation of inflammatory cytokines. Journal of Neuroinflammation. 2018. 15;15(1):320.
Moore C, Gupta R, Jordt SE, Chen Y*, Liedtke WB*. Regulation of Pain and Itch by TRP Channels. Neuroscience Bulletin. 2018. 34(1):120-142.
Rodriguez E, Sakurai K, Xu J, Chen Y, Toda K, Zhao S, Han BX, Ryu D, Yin H, Liedtke W, Wang F. A craniofacial-specific monosynaptic circuit enables heightened affective pain. Nature Neuroscience. 2017. 20(12):1734-1743.
Chen Y, Moore CD, Zhang JY, Hall RP 3rd, MacLeod AS, Liedtke W. TRPV4 Moves toward Center-Fold in Rosacea Pathogenesis. Journal of Investigative Dermatology. 2017.137(4):801-804.
Kanju P, Chen Y, Lee W, Yeo M, Lee SH, Romac J, Shahid R, Fan P, Gooden DM, Simon SA, Spasojevic I, Mook RA, Liddle RA, Guilak F, Liedtke WB. Small molecule dual-inhibitors of TRPV4 and TRPA1 for attenuation of inflammation and pain. Science Report. 2016. 1;6:26894.
Chen Y, Fang Q, Wang Z, Zhang JY, MacLeod AS, Hall RP, Liedtke WB. Transient Receptor Potential Vanilloid 4 Ion Channel Functions as a Pruriceptor in Epidermal Keratinocytes to Evoke Histaminergic Itch. Journal of Biological Chemistry. 2016. 6;291(19):10252-62.
Zhang Y, Chen Y*, Liedtke W*, Wang F. Lack of evidence for ectopic sprouting of genetically labeled Aβ touch afferents in inflammatory and neuropathic trigeminal pain. Molecular Pain. 2015. 10;11:18. (#=co-first author)
Lee W, Leddy HA, Chen Y, Lee SH, Zelenski NA, McNulty AL, Wu J, Beicker K, Coles J, Zauscher S, Grandl J, Sachs F, Guilak F, Liedtke W. Synergy between Piezo1 and Piezo2 channels confers high-strain mechanosensitivity to articular cartilage. Proceedings of the National Academy of Sciences. 2014; 111(47):E5114-22.
Chen Y, Kanju P, Fang Q, Lee SH, Parekh PK, Lee W, Moore C, Brenner D, Gereau RW, Wang F, Liedtke W. TRPV4 is necessary for trigeminal irritant pain and functions as a cellular formalin receptor. Pain. 2014; 155(12):2662-72.
Moore C, Cevikbas F, Pasolli A, Chen Y, Kong W, Kempkes C, Parekh P, Lee SH, Kontchou NA, Ye I, Jokerst NM, Fuchs E, Steinhoff M, Liedtke W. UVB radiation activates epidermal TRPV4 to trigger endothelin-1 signaling that generates photo-induced inflammation and pain. Proceedings of the National Academy of Sciences. 2013; 110(34):E3225-34.
Chen Y, Williams SH, McNulty AL, Hong JH, Lee SH, Rothfusz NE, Parekh PK, Moore C, Gereau RW, Taylor AB, Wang F, Guilak F, Liedtke W. Temporomandibular joint pain: A critical role for Trpv4 in the trigeminal ganglion. Pain. 2013; 154:1295-304. (Featured on Cover)
Chen Y*, Palm P, Lesch KP, Gerlach M, Moessner R, Sommer C. 5-hydroxyindolacetic acid (5-HIAA), a main metabolite of serotonin, is responsible for complete Freund's adjuvant-induced thermal hyperalgesia in mice. Molecular Pain. 2011; 7:21.
Chen Y*, Boettger K, Reif A, Schmitt A, Üceyler A, Sommer C. Inhibition of nitric oxide synthase modulates CFA-induced thermal hyperalgesia by cytokine regulation in mice. Molecular Pain. 2010; 6:13.
Willcockson HH, Chen Y, Han JE, Valtschanoff JG. Effect of genetic deletion of the vanilloid receptor TRPV1 on the expression of Substance P in sensory neurons of mice with adjuvant induced arthritis. Neuropeptides. 2010; 44:293-7.
Chen Y, Willcockson HH, Valtschanoff JG. Influence of the vanilloid receptor TRPV1 on the activation of spinal cord glia in mouse models of pain. Experimental Neurology. 2009; 220:383-90.
Chen Y, Willcockson HH, Valtschanoff JG. Vanilloid receptor TRPV1–mediated phosphorylation of ERK in murine adjuvant arthritis. Osteoarthritis and Cartilage. 2009; 17:244-51.
Chen Y*, Sommer C. The role of mitogen-activated protein kinase (MAPK) in morphine tolerance and dependence. Molecular Neurobiology. 2009, 40:101-7.
Chen Y, Willcockson HH, Valtschanoff JG. Increased expression of CGRP in sensory afferents of arthritic mice – effect of genetic deletion of the vanilloid receptor TRPV1. Neuropeptides. 2008; 42:551-6.
Chen Y*, Geis C, Sommer C. Activation of TRPV1 contributes to morphine tolerance: involvement of the MAPK signaling pathway. Journal of Neuroscience. 2008; 28:5836-45.
Palm F, Mössner R, Chen Y, He L, Gerlach M, Bischofs S, Riederer P, Lesch KP, Sommer C. Reduced thermal hyperalgesia and enhanced peripheral nerve injury after hind paw inflammation in mice lacking the serotonin-transporter. European Journal of Pain. 2008; 12:790-7.
Boettger MK, Uceyler N, Zelenka M, Schmitt A, Reif A, Chen Y, Sommer C. Differences in inflammatory pain in nNOS-, iNOS- and eNOS-deficient mice. European Journal of Pain. 2007;11:810-8.
Chen Y*, Sommer C. Activation of the nociceptin opioid system in rat sensory neurons produces antinociceptive effects in inflammatory pain: involvement of inflammatory mediators. Journal of Neuroscience Research. 2007; 85:1478-88.
Chen Y*, Sommer C. Nociceptin and its receptor in rat dorsal root ganglion neurons in neuropathic and inflammatory pain models: implications on pain processing. Journal of the Peripheral Nervous System. 2006; 11:232-40.
Yang Q, Chen Y, Fu CY, Chang M, Peng YL, Wang R. Effects of [Nphe1]nociceptin(1- 13)NH2,[Phe1(CH2-NH)Gly2]nociceptin(1-13)NH2, and nocistatin on nociceptin inhibited constrictions of guinea pig isolated bronchus. Protein and Peptide Letters. 2006; 13:185-8.
Chen LX, Fang Q, Chen Q, Guo J, Wang ZZ, Chen Y, Wang R. Study in vitro and in vivo of nociceptin/orphanin FQ(1-13)NH2 analogues substituting N-Me-Gly for Gly2 or Gly3. Peptides. 2004; 25: 1349-54.
Chen Y, Chang M, Wang ZZ, Chen LX, Yang Q, Qi YM, Wang R. [Nphe1]nociceptin(1-13)NH2 antagonizes nociceptin-induced hypotension, bradycardia and hindquarters vasodilation in the anesthetized rat. Canadian Journal of Physiology and Pharmacology. 2002; 80:31-5.
Chen LX, Wang ZZ, Wu H, Fang Q, Chen Y, Wang R. Effects of nociceptin (13-17) in pain modulation at supraspinal level in mice. Neuroscience Letters. 2002; 331:95-8.
Chen Y, Chang M, Wang R. Progress in the studies of nociceptin related peptides. Progress in Biochemistry and Biophysics. 2004; 31:106-11.
Chen LX, Chen Y, Peng YL, Wang ZZ, Chen Q, Wang R. Effects of nocistatin or nocistatin (10~17) on nociceptin in antagonizing endomorphin-1 and endomorphin-2 analgesia in mice. Acta Pharmacologica Sinica. 2002; 37: 837-40.
Chen Q, Chen Y, Chen LX, Yang DJ, Dong SL, Wang R. The effects of the synthetic nocistatin on blood vessel activities. Chinese Science Bulletin. 2001; 46:675-8.
Chen Y, Chen LX, Chen Q, Yang DJ, Peng YL, Yang Q, Wang R. Reversal by nocistatin of the effect of nociceptin in antagonizing morphine analgesia in mice. Chinese Pharmacology Bulletin. 2001; 17:383-5.
Media
In addition to the news stories published on our own Departmental website, Dr. Chen's expertise or research appears on the following stories on the following locations.
1. Scientists find new pain-suppression center in the brain (NIH)
2. Duke Anesthesiology awarded program project grant (Duke Department of Anesthesiology)
3. Facing Pain Head-On (National Institutes of Health)
5. Could discovery lead to end of sunburn pain? (Science Daily)