Duke Neurology 2022: A Year in Review (Part 1 of 2)
The Duke Neurology Department continued to grow and advance its missions of patient care, research, and training the next generation of neurology providers in 2022. Highlights from the first half of our calendar year include national and Duke-wide awards recognizing our faculty’s contributions to the field of diversity, inclusion, and neurology as a whole. The same period also saw the growth of the new Duke/UNC Alzheimer’s Disease Research Center and three of our neurologists don helmets and get in their racing care.
Duke Neurology Research Round Up, October 2022
Members of the Duke Neurology Department contributed to 12 new peer-reviewed journal articles published this September. Among other findings, this research answered important questions about the use of telehealth to manage chronic neurological conditions, investigated an alternative therapy’s potential benefit for fighting ALS, and synthesized the latest research findings about the role of the immune system and infection in the genesis of Alzheimer’s disease.
U.S. News & World Report ranks Duke University Hospital 23rd in nation for Neurology & Neurosurgery
U.S. News & World Report ranked Duke University Hospital as the top hospital in North Carolina and the 23rd best across the nation for neurology and neurosurgery in its 2022-2023 hospital rankings. The annual rankings, which assessed more than 4,500 hospitals nationwide, analyze and integrate dozens of medical and surgical services.
Faculty Spotlight: William Powers, MD
William Powers, MD, went to medical school with the intention of being the local doctor of a small New England town. The logical reasoning, intellect, and clinical showmanship of the then-Chair of Neurology Fred Plum got him hooked in neurology, however. Powers hasn't been bored in the five decades since. For this week’s Spotlight interview, Powers talks to us about how neurology has grown as a discipline since he was a resident.
Duke Neurology Research Round Up, June 2022
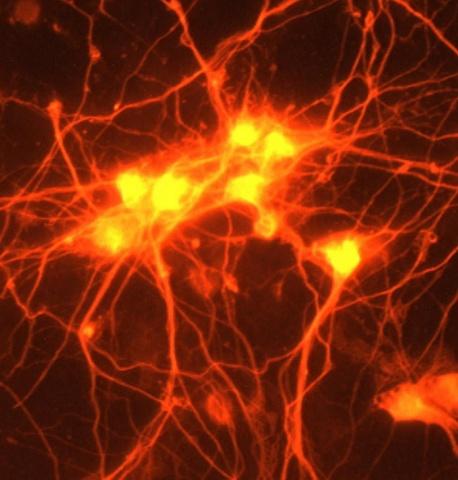
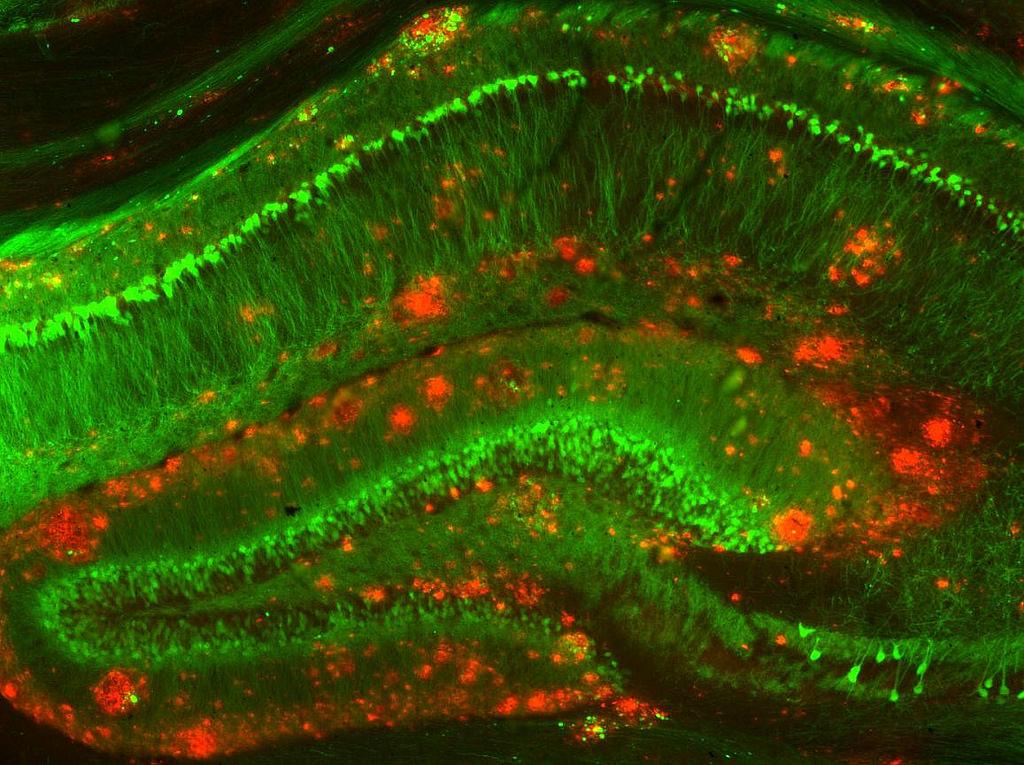
Members of the Duke Neurology Department contributed to 13 new peer-reviewed journal articles this May, advancing our understanding of how viruses that kill cancer cells may be used against brain tumors, the optimal treatments for various types of stroke, the origins of Parkinson’s disease, and more. Read the paragraphs below for summaries of our research from the past 31 days, as well as links to the complete articles themselves.
Hospital Neurology
Duke Neurology 2021: A year in review (part 2 of 2)
The second half of 2021 was as eventful as the first for the Duke Neurology Department. Story highlights from July through December of this year include our Leonard White, PhD, winning a national award for excellence in teaching, the founding of a joint Duke/UNC Alzheimer’s Disease Research Center, two of our hospitals receiving the American Heart Association/American Stroke Association’s highest award for quality stroke care, and the School of Medicine receiving awards totaling $18 million to uncover the origins of Parkinson’s disease.
Duke Neurology 2021: A year in review (part 1 of 2)
The Duke Neurology Department continued to grow and expand its missions of providing excellent clinical care, conducting research to improve our understanding of neurological conditions and how to treat them, and training the next generation of neurologists throughout 2021.
Faculty Spotlight: Adam Hartman, MD
Adam Hartman, MD, didn’t decide to specialize in neurology until the last year of medical school, but the puzzle-solving nature of the discipline, and the engaging, fast-paced tempo of acute neurology in particular, drew him in during his residency. Now, he’s one of our new neurohospitalists, where he’ll be treating complex cases in Duke Regional and Duke University Hospitals. For this week’s “Spotlight” interview, Hartman talks to us about why he loves hospital neurology, what he’s looking forward to over the next decade, and running and staying active when he’s not at Duke.
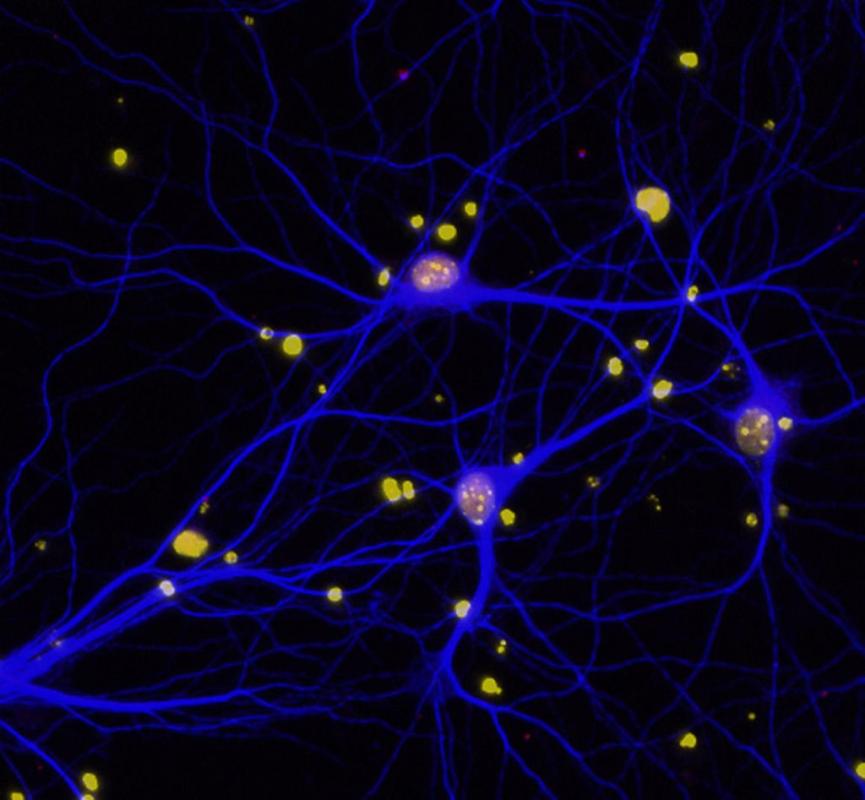
Duke Neurology Research Round Up, July 2021
New publications written by members of the Duke Neurology Department published this June advanced our understanding of the origins of Alzheimer’s disease, stroke, and spinal injuries, as well as offering new insights on how to better diagnose and treat these and other conditions. Our faculty contributed to recent articles in Lancet Neurology, Stroke, and other high-impact journals. Read more about each of these stories, and find links to the original articles themselves, in the paragraphs below.
Neuromuscular Disease
New Neurology division brings consultative care to diverse inpatient settings
A patient hospitalized for a heart attack may suddenly have a stroke. A patient hospitalized with a metastatic tumor may suddenly have a seizure. Providers within Duke’s new division of Hospital Neurology specialize in helping patients with complex, overlapping conditions across all three Duke hospitals.
In this Q&A, division chief Matthew W. Luedke, MD, discusses this expanded approach to patient care and how neurohospitalists can help fill gaps in inpatient and outpatient settings.