Faculty Spotlight: Michael Morris, MD
Michael Morris, MD, first found himself drawn to neurology shortly after starting his clinical rotations as a medical student. Later, he decided to specialize in neurocritical care after experiencing the acuity and hands-on nature of the specialty. Now, he’s the newest member of our neurocritical care team, where he works to help individuals with life-threatening illnesses within our Neuro-Intensive Care Unit.
Duke Neurology Research Round Up, September 2022
Members of the Duke Neurology Department contributed to 12 new peer-reviewed journal articles published this August. Highlights include a review article examining evoked potentials used for deep brain stimulation in Parkinson’s, the healthcare received by veterans with epilepsy, the optimal stroke treatments for patients with cerebral venous thrombosis, and other topics.
Duke Neurology Research Round Up, August 2022
Members of the Duke Neurology Department contributed to eight articles and two correspondence letters published in peer-reviewed journals this July.
U.S. News & World Report ranks Duke University Hospital 23rd in nation for Neurology & Neurosurgery
U.S. News & World Report ranked Duke University Hospital as the top hospital in North Carolina and the 23rd best across the nation for neurology and neurosurgery in its 2022-2023 hospital rankings. The annual rankings, which assessed more than 4,500 hospitals nationwide, analyze and integrate dozens of medical and surgical services.
Duke Neurology Research Round Up, June 2022
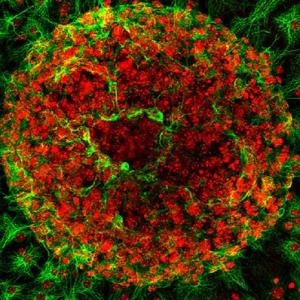
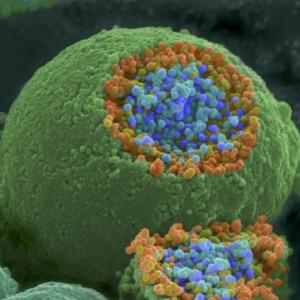
Members of the Duke Neurology Department contributed to 13 new peer-reviewed journal articles this May, advancing our understanding of how viruses that kill cancer cells may be used against brain tumors, the optimal treatments for various types of stroke, the origins of Parkinson’s disease, and more. Read the paragraphs below for summaries of our research from the past 31 days, as well as links to the complete articles themselves.
Hospital Neurology
APP Spotlight: Cherith Godwin, MSN, AGACNP-BC
Cherith Godwin comes from a family of nurses, but hesitated to enter the field herself. Fortunately, she reconsidered and is now a member of our neurocritical care team in our neuro intensive care unit (Neuro ICU).
Duke Neurology Research Round Up, April 2022
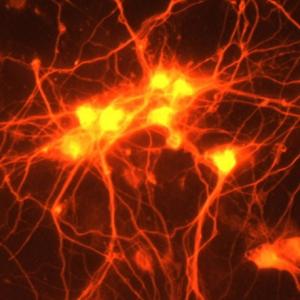
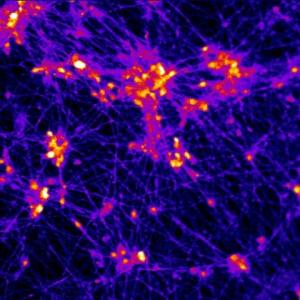
This March, members of our Department contributed to studies that reveal potential new therapeutic targets for Alzheimer’s disease, help triage patients suffering from traumatic brain injury, address issues contributing to physician burnout, and more. In all, our faculty, staff, students, and trainees contributed to 15 studies published over the past 31 days. Read about them and find links to the original articles below.
Parkinson’s and Movement Disorders
Duke Neurology Research Round Up, February 2022
The first month of 2022 saw the publication of 18 new peer-reviewed journal articles from members of the Duke Neurology Department. Highlights include a new article in Lancet Neurology discussing the epidemiology, diagnostics, and biomarkers of autoimmune neuromuscular junction disorders, case reports describing the progression and treatment options for rare neurological conditions, and a summary of how the first year of the COVID-19 pandemic affects neurology residency programs in the United States.
APP Spotlight: Emily Elfreich, ARNP
For Emily Elfreich, ARNP, taking care of some of Duke University Hospital’s most critical patients is all in a day’s (or a night’s) work. The nurse practitioner diagnoses, assesses, and treats patients in our Neuro Intensive Care Unit (Neuro ICU) in 12 and 24 hour shifts. In this week’s “Spotlight” interview, Elfreich talks to us about thriving in a busy, high-stress environment, her career path in nursing, and enjoying traveling, her rescue dogs, and reality television as stress relievers outside of work.
Duke Neurology 2021: A year in review (part 2 of 2)
The second half of 2021 was as eventful as the first for the Duke Neurology Department. Story highlights from July through December of this year include our Leonard White, PhD, winning a national award for excellence in teaching, the founding of a joint Duke/UNC Alzheimer’s Disease Research Center, two of our hospitals receiving the American Heart Association/American Stroke Association’s highest award for quality stroke care, and the School of Medicine receiving awards totaling $18 million to uncover the origins of Parkinson’s disease.