The Duke Center for Research in Autoimmunity and Multiple Sclerosis (DREAMS) is a multidisciplinary group of basic and clinical researchers dedicated to improving our understanding of, and patient care for, MS and autoimmune disease (AI). Your gift to DREAMS can help fund this much-needed research.
About DREAMS
DREAMS allows researchers throughout Duke to collaborate, facilitate novel research by the provision of seed funding, and improve education awareness and outreach of MS and auto-immune (AI) diseases. Established in 2015, DREAMS includes 19 faculty members from 7 departments within the Duke School of Medicine.
Investigators from the basic sciences are studying AI- and MS-related topics including model systems of disease pathology, immune cell regulation and function, re-myelination, and the role of environmental factors such as diet on MS and AI diseases. Our clinical research includes the neuroimmunological mechanisms associated with diseases including paraneoplastic syndrome, myasthenia gravis, and pediatric infectious disease, while further characterizing the pathoetiology of MS and its subtypes. An additional underpinning of DREAMS is its investment in clinical and patient education, as well as the initiation of a dedicated LP clinic that will collect cerebrospinal fluid for future MS and AI research.
Simon Gregory, PhD, Director of Research
Simon Gregory and his collaborators were the first to identify genetic association of a MS gene outside of the MHC. Gregory is also Principal Investigator of the MURDOCK-MS study, a 1,000 patient MS collection that aims of understanding the mechanisms associated with MS development and progression, and the generation of multi-omic biomarkers to facilitate reclassification of the disease.
Christopher Eckstein, MD, Co-Director of Research
Christopher Eckstein, MD joined the clinical staff at the Duke Neurology Department in 2015 and co-developed the DREAMS concept with Simon Gregory, PhD, and Department of Neurology chair, Richard O’Brien, MD, PhD later that year. Dr. Eckstein’s clinical research interest is associated with Autoimmune Encephalopathies specifically their diverse clinical manifestations and therapeutic response. Eckstein has recently developed a lumbar puncture clinic at Duke who goal, in addition to providing material for diagnosis, is to bank CSF for future research by DREAMS faculty.
Mark Skeen, MD Director of Clinical Research and Education
Mark Skeen, MD, collaborates with researchers within DREAMS, the Duke Clinical Research Institute, and other organizations to establish new directions for research, and act as an ambassador for DREAMS and to identify and recruit study participants to clinical trials and basic research within Duke.
F. Lee Hartsell, MD, MPH, Director of Connected Health
F. Lee Hartsell’s clinical interests include CNS inflammatory demyelinating diseases including MS, neuromyelitis optica and transverse myelitis. In addition to research interests of emerging MS therapies and understanding the role of Vitamin D in MS, Dr. Hartsell has been collaborating with Katherine Heller to develop an MS iPhone app that uses machine learning and mobile technology to classify of daily MS patient symptoms, engage and educate users, and aggregates symptom patterns for patients and their providers.
As directors of clinical research, Mark Skeen, MD, and Chris Eckstein, MD collaborate with researchers within DREAMS, the Duke Clinical Research Institute, and other organizations. They help to identify and recruit study participants, establish new directions for research, and act as an ambassador for DREAMS by convincing researchers within Duke to join the project.
Mark Skeen, MD – Director of Clinical Research
Chris Eckstein, MD - Associate Director of Research
Neuroimmunology
- John Yi, PhD (Surgery) – Myasthenia gravis immune profiling Rehabilitation/Traumatic brain injury
Traumatic Brain Injury and Neurorehabilitation
- Joel Morgenlander, MD (Neurology) - Sports concussion and traumatic brain injury
- Jodi Hawes, MD (Neurology) - Stroke, traumatic brain injury, neurorehabilitation neuro-
Opthalmology
- Mays Antoine El-Dairi, MD (Opthamology):
- MS and ophthalmic manifestations
-
monitoring ophthalmic manifestations in adult and pediatric intracranial hypertension
-
monitoring eye deformation in high intracranial pressure (ICP)
-
monitoring vision and optic nerves in babies with neurologic disease from prematurity or hypoxic ischemic encephalopathy
Neuro-Radiology
- James Provenzale, MD - design and implementation of nanoparticles
Pediatrics
- Heather Van Mater, MD, MS - Pediatric AI diseases (RA)/Autoimmune encephalitis
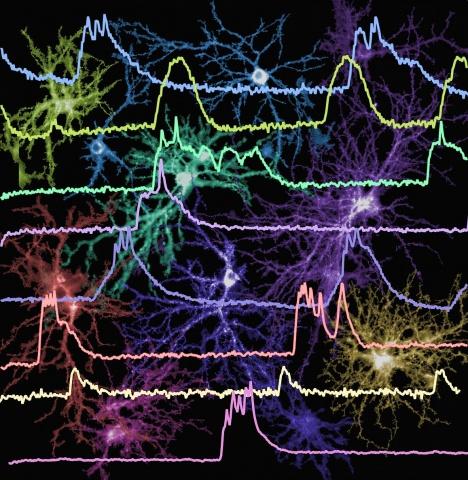
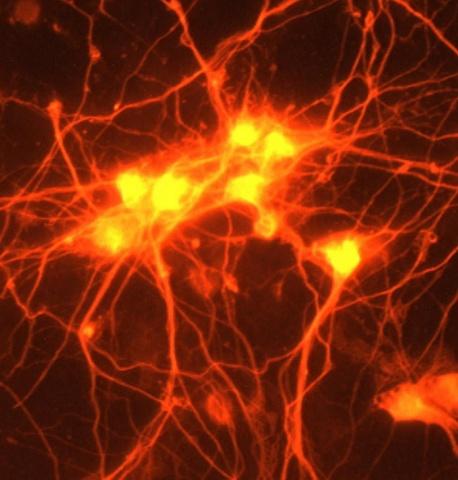
DREAMS' basic research faculty seeks to improve our understanding of the origins and progression of MS and AI disease, as well as the body's response to the condition and treatment, examining new imaging techniques, specific elements of the body's immune response, the condition of neuronal myelin over time, and how nutrition affects disease progression.
Genomics and Epigenetics:
- Simon Gregory, PhD (Neurology, Medicine, and Molecular Genetics and Microbiology)
Imaging:
- Glen Jaffe, MD (Opthamology) – OCT/MVEP
Immunology:
- Mari Shinohara, PhD (Immunology) – Model systems of EAE and inflammation
- Maria Ciofani, PhD (Immunology) – Th17 lineage, fate mapping and regulation
- Thomas Tedder, PhD (Immunology) – B-cells and EAE, Lymphoma, NMO spectrum disorder
- Kent Weinhold, PhD (Surgery) - Immunologic signatures of disease, monitoring of immune checkpoint blockade
- Dennis Ko, MD, PhD (Molecular Genetics and Microbiology) – Immunology of host response
De/remyelination:
- Eric Benner, MD, PhD (Pediatrics) – White matter injury
Nutrition and Immunity:
- Nancie MacIver, MD, PhD (Pediatrics) – Diet and Inflammation
To facilitate research and patient education, DREAMS funds monthly journal clubs and quarterly dinners, bursaries for trainee education, and seed funding for novel high-risk, high-reward research that will transform our understanding of MS and AI, and which will be translated into larger government and foundation-sponsored research. Give to DREAMS here.